Typhoid toxin aids survival in mice
Bacterial protein prolonged life of infected host animals with no increase in cancer
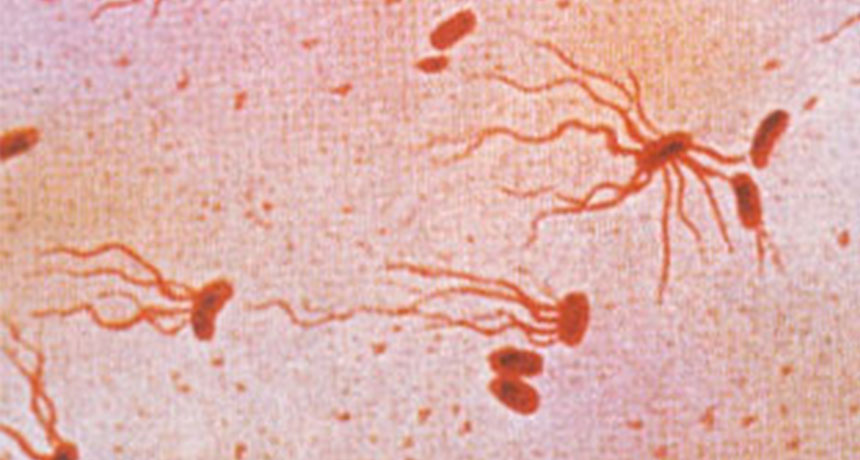
TOXIN TANKS The bacterium Salmonella enterica Typhi causes typhoid fever in humans and produces a DNA-damaging protein called typhoid toxin. Typhoid toxin appears to prolong survival and reduce gut inflammation in S. enterica-infected mice, a new study suggests.
Roinujs/Wikimedia Commons
- More than 2 years ago
A DNA-damaging protein in typhoid bacteria might keep infected animals alive and provide a safe haven for the microbes.
Typhoid toxin, a protein produced by the typhoid fever-causing bacterium Salmonella enterica Typhi, tears DNA molecules apart. But the protein actually prolonged survival and reduced gut inflammation in mice infected with S. enterica, an international team of researchers reports April 7 in PLOS Pathogens.
The deadly, mouse-infecting version of S. enterica doesn’t normally make the typhoid toxin. So the scientists modified mouse S. enterica with typhoid toxin genes from the human-infecting strain responsible for the high fever, headache and rash of typhoid fever. The team thought that typhoid toxin’s DNA slashing might cause tumors, but in mice fed the toxin-making S. enterica, no increased cancer risk appeared compared with mice given the toxin-free microbes. To the researchers’ surprise, though, more mice with the toxin survived 20 days of infection than did mice with the toxin-free strain.
“When I first saw the data on the survival of the mice, I said, ‘No, we mixed up the strain,’ because we were expecting exactly the opposite,” says study coauthor Teresa Frisan, a cellular microbiologist at the Karolinska Institute in Stockholm. “We were chasing cancer, and we found biology of the toxin.”
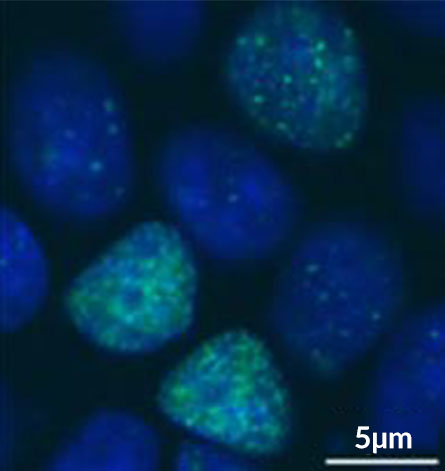
Mice infected with the typhoid toxin-making strain also had less intestinal inflammation after 10 days. Several genes linked to inflammation and immunity became less active after exposure to the toxin-making microbes, the team found. “Basically, what this toxin does is it modulates the host immune response,” Frisan says. This effect varied in other organs, with mouse livers showing increased inflammation regardless of the bacterial strain.
Increased survival and decreased immunity may extend S. enterica’s stay within its host’s body. After six months, mice that survived infection with the typhoid toxin-free strain had no detectable S. enterica in their livers. But five out of six mice infected with the toxin-making strain still had substantial amounts of the bacteria in their livers. These results suggest that typhoid toxin promotes long-term, symptom-free infections, the researchers say.
“Bacteria don’t want to kill their host; that makes no good sense,” says microbiologist Bradley Jones of the University of Iowa’s Carver College of Medicine in Iowa City. “You want to establish a low-level infection in your host, and then you just basically can grow … and you don’t have to go through this constant fighting for resources.” It appears that bacteria use typhoid toxin to ward off attacking immune cells, Jones says.
Distinct differences exist between the mouse-infecting and human-infecting strains of S. enterica, even with the modifications made in the study, Jones says. Such differences could limit the clinical applicability of the results. But future studies could explore the possibility of disabling typhoid toxin to bolster an infected animal’s immune defenses, Jones says.
Frisan says the scientists next hope to figure out exactly how typhoid toxin and its DNA-breaking action manipulate a host’s immune system. But given the toxin’s apparent ability to keep infected animals alive — and infectious bacteria around — the team suggests that the label of “toxin” may actually be undeserved.