Is the coronavirus mutating? Yes. But here’s why you don’t need to panic
Lab experiments would help determine whether mutations change how the virus infects cells

Viruses are always changing, acquiring small mutations in their genetic material over time as they spread among people. While those changes help researchers track the coronavirus’s path around the globe, they don’t often alter how the virus works.
T. Tibbitts
In novels and movies, infectious pathogens mutate and inevitably become more dangerous. In the blockbuster movie Contagion, for instance, a deadly virus acquires a mutation in Africa that causes the global death toll to spike in mere days.
Reality, however, is far less theatrical.
Over the past few months, a few research groups have claimed to identify new strains of the coronavirus, called SARS-CoV-2, that’s infecting people around the globe. That sounds scary. But not only is it sometimes difficult to determine whether a change amounts to a “new strain,” none of the reported changes to the virus have been shown to make it more dangerous.
This has led to great confusion for the general public. Each time such studies surface, fears arise, and virus experts rush to explain that changes in a virus’s genetic blueprint, or genome, happen all the time. The coronavirus is no exception.
“In fact, it really just means that it’s normal,” says Kari Debbink, a virologist at Bowie State University in Maryland. “We expect viruses to evolve. But not all of those mutations are meaningful.”
Here’s what it means to find mutations in the novel coronavirus, and what evidence is needed to actually raise a red flag.

Trustworthy journalism comes at a price.
Scientists and journalists share a core belief in questioning, observing and verifying to reach the truth. Science News reports on crucial research and discovery across science disciplines. We need your financial support to make it happen – every contribution makes a difference.
First, a mutation is just a change
Most of the time, mutations don’t do anything to a virus at all.
Viruses are simply protein shells that contain either DNA or RNA as their genetic material. In the case of SARS-CoV-2, it’s RNA. The building blocks of RNA, called nucleotides, are arranged in triplets, called codons. These nucleotide trios provide the code for building amino acids, which make up the virus’s proteins. A mutation is a change to one of these nucleotides in the virus’s genetic material — in SARS-CoV-2’s case, one of around 30,000 nucleotides.
Sometimes a mutation in a triplet is silent, meaning the codon still codes for the same amino acid. But even when an amino acid does change, the virus might not behave in a way that’s obviously different. Some mutations could also spawn dysfunctional viruses that quickly disappear as a result.
And in fact, these changes can actually be helpful when it comes to tracing the virus’s path around the globe, something researchers have been doing ever since experts from China released the first coronavirus genetic sequence in January (SN: 2/13/20). Scientists can decipher, or sequence, the virus’s RNA to track changes as it infects more people. They can then track where and how the coronavirus is spreading in a population, and monitor for further changes in its genetics.
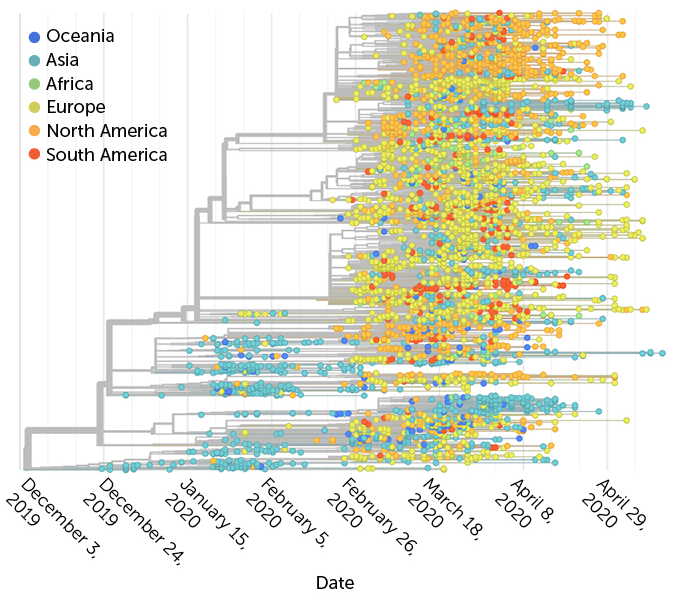
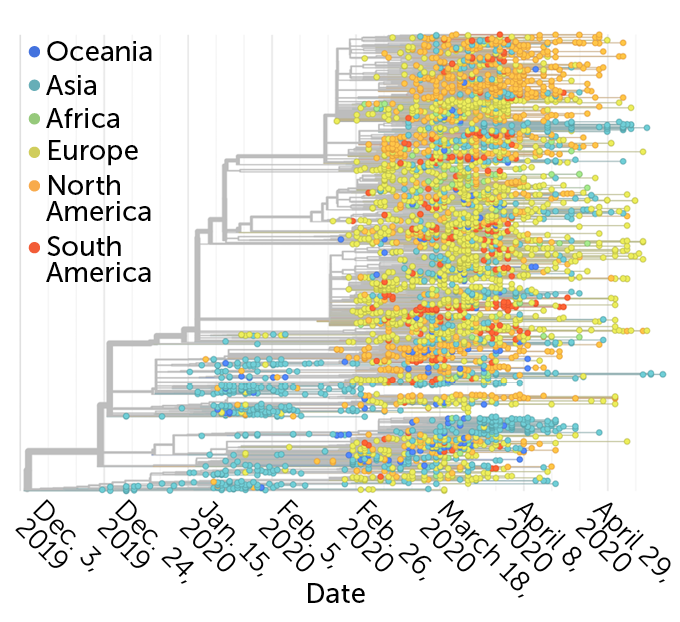
Close relatives
Researchers can use changes in the coronavirus’s genetic blueprint to better understand how it is spreading. By deciphering viruses taken from patients, they can build a tree (pictured, samples are represented by dots and colored by region where they were collected) to show the genetic relationships among those viruses. The pandemic got its start in China at the end of 2019 (blue circles at the bottom) and has since expanded to five other continents. The horizontal lines depict how closely related two viruses are — longer lines mean there are more differences between them.
Tracking SARS-CoV-2’s genetic changes to map its spread, December 2019–May 2020
Epidemiologists are interested in tracking mutations even if they don’t alter the protein, says Emma Hodcroft, a molecular epidemiologist at the University of Basel in Switzerland. “But that doesn’t mean that it’s a new strain or that it’s a virus that behaves differently.”
A new ‘strain’ of virus doesn’t mean much
The term “strain” is “used very, very loosely by most scientists,” Hodcroft says. “There isn’t really a strict definition of the word ‘strain,’” particularly when talking about viruses. Experts might simply be referring to viruses that aren’t genetically identical — almost like discussing different people.
Viruses are always changing. When a virus infects a cell, it begins making copies of its genetic instructions. Most viruses don’t have the necessary tools to proofread each string of RNA for mistakes, so the process is error-prone and differences build up over time.
Coronaviruses like SARS-CoV-2, on the other hand, do have a proofreading enzyme — a rarity for RNA viruses. But that doesn’t mean their genomes don’t have errors. Changes still accumulate, just more slowly than in other RNA viruses such as influenza. “Strains,” “variants” or “lineages” are all terms researchers might use to describe viruses that have identical or closely related strings of RNA.
But for the general public, a word like “strain” is often interpreted to mean a whole new scourge. “I think the use of the term ‘strain’ does little more than cause panic,” says Jeremy Luban, a virologist at the University of Massachusetts Medical School in Worcester. “It doesn’t really get at what the important issues are.”
Most mutations aren’t dangerous
A mutation can affect a virus in a number of ways, but only certain kinds of mutations might make the virus more dangerous to people. Perhaps the change shields the virus from the immune system, or makes it resistant to treatments. Mutations could also alter how easily the virus spreads among people or cause shifts in disease severity.
Luckily, such mutations are rare. Unfortunately, they can be hard to identify.
A preliminary study published May 5 at bioRxiv.org, for instance, found a mutation in the SARS-CoV-2 spike, a protein on the outside of the coronavirus that allows it to break into cells. This new variant is now found more often in places like Europe and the United States than the original form of the coronavirus. That may mean the change makes the virus more transmissible, the authors concluded. But the study lacked laboratory experiments to support the claim.
Other explanations could also explain the pattern. The SARS-CoV-2 variant with the mutation could have ended up in certain regions thanks to random chance — a person infected with a virus that had the new mutation just happened to hop on a plane — and might have nothing to do with the virus itself. The study didn’t provide enough evidence to distinguish among the possibilities.
“What I think has been potentially confusing to people is that we’re watching this very normal process of [viral] transmission and mutation happen in real time,” says Louise Moncla, an evolutionary epidemiologist at the Fred Hutchinson Cancer Research Center in Seattle. “And there’s this real desire to understand whether these mutations have any functional difference.”
‘Take a deep breath,’ experts say, and expect mutations
To understand whether a single mutation changes how the virus works, “it’s not just going to be one experiment,” Bowie State virologist Debbink says. “It takes a lot of research.”
In addition to examining genetic sequences of viruses from coronavirus patients all over the world, researchers will also rely on studies in lab-grown cells or animals. Such studies could help pinpoint whether viruses with particular mutations behave differently. Competition experiments — where two different viruses are mixed in cells in a dish or used to infect an animal — can help scientists figure out which variant is more successful at making copies of itself, that is, which one “wins.”
Other types of tests could reveal if mutations in the coronavirus’ spike protein alter how strongly it attaches to the protein on human cells that allows it to get inside the cells, virologist Luban says (SN: 2/3/20), or whether changes modify how easily the virus gets into a cell after binding.
But lab results might not provide the full picture either. “Just because something’s different in a cell doesn’t necessarily mean that it’s different when you scale that up to the whole human body,” Hodcroft says. “At the end of the day, you’re going to need some animal studies or some really good human data.”
These studies take time. Meanwhile, more coronavirus mutations are guaranteed to pop up over the coming months — and experts will continue to track them.
“The data will tell us whether we need to worry, and in what way we need to worry,” Moncla says. “Everyone should take a deep breath and realize that this is exactly what we’ve always expected to happen, and we don’t necessarily need to be concerned.”
Sign up for our newsletter
We summarize the week's scientific breakthroughs every Thursday.