Defusing the Dairy Dilemma
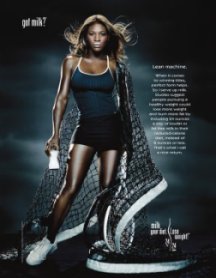
There can’t be many people who have missed the national “Got Milk?” ads of the past decade. This whimsical campaign for U.S. dairies has featured some 200 celebrities, athletes, and musicians sporting exaggerated milk mustaches. The Milk Processor Education Program has said its goal in the ads has been to show that consuming milk is cool (not just for babies any more) and healthy. The cited benefits include strengthening bones and teeth, lowering blood pressure, and limiting weight gain.
However, increasing the consumption of milk by teens and adults has proven an uphill battle, particularly among people who have—or suspect they have—lactose intolerance.
Beginning around age 2, as much as three-quarters of people around the world lose their ability to produce ample lactase. That’s the enzyme needed to break down lactose, the primary sugar in milk.
When these lactose-intolerant individuals consume dairy products, most of milk’s sugar will pass largely undigested through the upper gastrointestinal tract and into the colon. That’s not good because there, normal, gut-dwelling microbes will feast on the sugar and belch out hydrogen and other gases. Indeed, researchers test for lactose intolerance by measuring hydrogen in a person’s breath after a meal.
When a person with intolerance consumes too much milk or cheese, a host of unpleasant symptoms can arise: chiefly nausea, cramps, flatulence, and diarrhea.
As many as 50 million people in the United States are considered lactose intolerant, with certain ethnic groups disproportionately affected. Some 80 percent of African Americans and Native Americans have the condition, as do more than 90 percent of Asian Americans. In contrast, only about 10 percent of adults with a Northern-European heritage have trouble breaking down lactose.
However, a new analysis in the Journal of Nutrition finds that even people with confirmed lactose intolerance can usually drink at least a cup of milk without symptoms—especially if that milk is consumed with a meal. The finding didn’t surprise human nutritionist Dennis A. Savaiano of Purdue University, the study’s lead author. Indeed, it dovetailed with results from a host of clinical studies carried out by his team over more than a decade.
These data reinforce that people with lactose intolerance can safely digest more dairy than they think they can, says Savaiano, a lactose-intolerant Italian-American. Indeed, the researcher regularly drinks milk with breakfast and dinner and downs additional dairy foods most days during lunch. The trick is to consume them in moderation, he says.
Few people need to shun milk, one of the diet’s richest sources of calcium, says Savaiano. He points out that this mineral remains woefully deficient in most adults’ diets.
Got calcium?
Despite the recommendation that people age 6 and older consume between 1,000 and 1,500 milligrams of calcium daily, few adults do so.
Theresa Nicklas of the Department of Agriculture’s Children’s Nutrition Research Center in Houston has been studying the problem. At a biology meeting last year, she and her colleagues reported that in Bogalusa, La., 80 percent of a population of adults consume no more than two servings of milk or other dairy foods per day. About half of the study participants consumed one serving or less. Considering that a cup of milk has only 300 mg of calcium, few people were deriving much of the mineral from dairy sources.
Other foods containing calcium don’t fill the mineral gap for most people. Broccoli is a calcium-rich vegetable, but a typical serving of that has only 50 milligrams. The same amount of the mineral is present in a serving of enriched orange juice. A cup of soybeans or baked beans delivers more calcium—but still only half as much as a serving of milk does.
It’s because milk and other dairy products are such rich calcium sources that most nutritionists advocate consuming low-fat dairy products on a daily basis.
Overcoming intolerance
The Purdue researchers almost 2 decades ago began pursuing ways to help lactose-intolerant individuals cope with dairy foods. The team’s original ideas included keeping portion sizes small and eating them along with foods to slow the passage of milk sugar through the gut.
However, notes Savaiano, along the way his group and others found that many people who know they’re lactose intolerant—or think they are—are reluctant to consume dairy products at all. This is despite the fact that when tested, few people can tell the difference—in terms of symptoms—between foods free of lactose and those with a moderate amount.
Since most such studies have been small, the Purdue group decided to pool results from a host of experiments in which people were given a food with or without lactose and asked to record any gastrointestinal symptoms. In these trials, neither the participants nor researchers knew who got lactose-containing meals until after the tests had been completed.
Although a scan of the published record for potentially applicable studies turned up 1,553 possible candidates, independent reviewers dismissed most of them as containing either potential biases or major deficiencies in their design or data reports. In the end, Savaiano says, “I was surprised” at the small number of quality studies available for analysis. Just 21 met the criteria for inclusion.
In the April Journal of Nutrition, Savaiano’s team reports that among people diagnosed with lactose intolerance, the severity of symptoms is no worse after downing a cup of milk—or other food with an equivalent amount of lactose—than after ingesting a lactosefree food or drink. “This included perceived severity of abdominal bloating, abdominal pain, degree of loose stools or diarrhea and flatulence,” the team reports.
Although dose can make a big difference in whether symptoms appear, the researchers couldn’t gauge how big a difference from these studies because most had administered about the same amount of lactose.
Eating well, doing good
Savaiano’s team first reported its findings a year ago at a small symposium entitled Calcium-Related Chronic Diseases in Ethnic Minorities—Can Dairy Consumption Reduce Health Disparities? At the same meeting, Molly E. Reusser of Academic Network in Portland, Ore., and David A. McCarron of the University of California, Davis reviewed data on hypertension. They noted that blacks have far higher rates of high blood pressure than do whites. This major risk factor for heart disease currently afflicts at least 42 percent of all African American adults, more than 9 million people.
One diet that has proven effective at lowering blood pressure, especially in black adults, is known as DASH, for Dietary Approaches to Stop Hypertension. Although media attention has focused on the fruit-and-vegetable component of the regimen, Reusser and McCarron argue that this emphasis has been “both misplaced and misleading.” Why? The dietary elements that probably decreased blood pressure most were vitamin D and several minerals, including calcium, say the two researchers. A second study has also linked these nutrients and lowered blood pressure, they note.
Further analyses of the DASH study show that among several diets tested, one also cut two additional heart-disease risk factors, blood concentrations of folate and homocysteine. That diet, containing three daily servings of dairy foods, was the only one that “produced favorable changes” in the study participants, report Reusser and McCarron.
Robert P. Heaney of Creighton University noted at the 2005 symposium that at least when it comes to building bone, blacks tend to use calcium more efficiently than white people do. In other words, African Americans build stronger bones with smaller inputs of the mineral. However, since bone is far from the only tissue that benefits from calcium, even black people with healthy bones can’t assume they’re getting sufficient calcium. Indeed, said Heaney, a system within a black person’s body that protects bones even when calcium intake is low may actually increase that individual’s risk of obesity, heart disease, and diabetes
.
| Age | Recommended daily calcium intake |
| 0–6 months | 400 mg |
| 6–12 months | 600 mg |
| 1–5 years | 800 mg |
| 6–10 years | 1,200 mg |
| 11–24 years | 1,200–1,500 mg |
| 19–50 years | 1,000 mg |
| 51 years and up | 1,500 mg |
Inst. of Medicine







