Protein linked to Parkinson’s travels from gut to brain
Study in mice traces path of alpha-synuclein
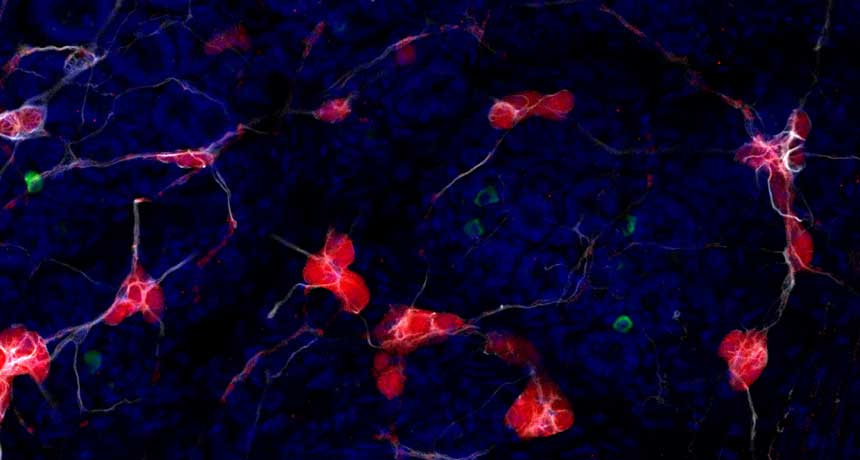
SEE-THROUGH VIEW Using a method that rendered tissue translucent, researchers were able to see alpha-synuclein clumps (green) in the gut of a mouse intermingled with nerve cells (red) and astrocytes (white). Cell nuclei are blue.
Collin Challis, Gradinaru Group/Caltech
SAN DIEGO — Over the course of months, clumps of a protein implicated in Parkinson’s disease can travel from the gut into the brains of mice, scientists have found.
The results, reported November 14 at the annual meeting of the Society for Neuroscience, suggest that in some cases, Parkinson’s may get its start in the gut. That’s an intriguing concept, says neuroscientist John Cryan of the University College Cork in Ireland. The new study “shows how important gut health can be for brain health and behavior.”
Collin Challis of Caltech and colleagues injected clumps of synthetic alpha-synuclein, a protein known to accumulate in the brains of people with Parkinson’s, into mice’s stomachs and intestines. The researchers then tracked alpha-synuclein with a technique called CLARITY, which makes parts of the mice’s bodies transparent.
Seven days after the injections, researchers saw alpha-synuclein clumps in the gut. Levels there peaked 21 days after the injections. These weren’t the same alpha-synuclein aggregates that were injected, though. These were new clumps, formed from naturally occurring alpha-synuclein, that researchers believe were coaxed into forming by the synthetic versions in their midst.
Also 21 days after the injections, alpha-synuclein clumps seemed to have spread to a part of the brain stem containing nerve cells that make up the vagus nerve, a neural highway that connects the gut to the brain. Sixty days after the injections, alpha-synuclein had accumulated in the midbrain, a region packed with nerve cells that make the chemical messenger dopamine. These are the nerve cells that die in people with Parkinson’s, a progressive brain disorder that affects movement.
After reaching the brain, alpha-synuclein spreads thanks in part to brain cells called astrocytes, a second study suggests. Experiments with cells in dishes showed that astrocytes can store up and spread alpha-synuclein among cells. That work was presented by Jinar Rostami of Uppsala University in Sweden at a news briefing on November 14.
The gradual accumulation and spread of alpha-synuclein caused trouble in the mice. As alpha-synuclein clumps slowly crept brainward, the mice began exhibiting gut and movement problems. Seven days after the injections, the mice’s stool was more plentiful than usual. Sixty and 90 days after the injections — after clumps of alpha-synuclein had reached the brain — the mice performed worse on some physical tests, including getting a sticker off their face and flipping around to shimmy down a pole headfirst. In many ways, the mice resembled other mice that have mutations that cause Parkinson’s-like symptoms, Challis says.
An earlier study turned up evidence that clumps of alpha-synuclein can move from the gut to the brain stem in rats, but those experiments looked at shorter time scales, Challis says. And previous work monitored the movements of the injected alpha-synuclein, as opposed to the alpha-synuclein clumps that the mice produced themselves.
The idea that alpha-synuclein can spread from the gut to the brain is very new, says Alice Chen-Plotkin, a clinician and Parkinson’s researcher at the Hospital of the University of Pennsylvania. These new results and others have prompted scientists to start looking outside of the brain for the beginning stages of the disease, she says. “Increasingly, people are wondering if it starts earlier.”
Some evidence suggests that the gut is a good place to look. People with Parkinson’s disease often suffer from gut problems such as constipation. And in 2015, scientists reported that a group of Danish people who had their vagus nerves severed were less likely to develop Parkinson’s disease. Cut alpha-synuclein’s transit route from the gut to the brain, and the disease is less likely to take hold, that study hints.
It’s not clear why alpha-synuclein accumulates in the gut in the first place. “There are a lot of theories out there,” Challis says. Bacteria may produce compounds called curli that prompt alpha-synuclein to aggregate, a recent study suggests. Pesticides, acid reflux and inflammation are other possible culprits that could somehow increase alpha-synuclein clumps in the gut, Challis says.