Is aging without illness possible?
Geroscientists are pursuing potential drugs that could expand health span

By addressing the root causes of aging, geroscientists hope to stave off the disability and diseases that can make old age so miserable.
Sam Chivers
Each morning after breakfast, Scott Broadbent takes a plastic bottle from the refrigerator in his home in Alameda, Calif., pops the top, and drinks the contents, 2.5 ounces of milky liquid. “It has sort of a pineapple creamy flavor,” he says. “It’s really not bad.”
The bottle might contain ketone ester, a supplement meant to help the body burn fat instead of carbohydrates. Researchers are now testing whether it might also slow the aging process. Or Broadbent might instead be getting a placebo. He is part of a clinical trial at the nearby Buck Institute for Research on Aging to assess the supplement’s safety and side effects in older adults.
A retired chemist who used to work for pharmaceutical companies, Broadbent is 70 and in excellent health today, but he worries about the future. He’s not necessarily afraid of dying, but he doesn’t want to be sick and in pain as he grows older. His dad had Parkinson’s disease. Broadbent survived prostate cancer and recently developed tinnitus, which spooked him and sparked anxiety attacks. “I thought if I had to live like this the rest of my life, I don’t know if I’d want to do it,” he says.
Some scientists think there’s a better way. These researchers — part of a burgeoning field called “geroscience” — aren’t seeking immortality. The focus is much more pragmatic: By addressing the root causes of aging, they hope to stave off the disability and diseases that can make old age so miserable. They want to help people feel healthy for longer, compressing the years of illness that often accompany old age into a much shorter time frame. “Let’s build a medicine that would be safe enough for someone in midlife to take almost like a supplement, like a daily vitamin, but with much more profound biological effects,” says James Peyer, CEO of Cambrian Bio in New York City.
Just don’t call these potential medicines antiaging therapies. “That term is associated with an industry that is trying to sell products to the public to separate people from their money,” says S. Jay Olshansky, a demographer and geroscientist at the University of Illinois Chicago. The antiaging market includes everything from face creams meant to zap wrinkles to pills that promise to turn back the clock. “It’s bogus,” he says. Geroscientists instead are doing legitimate research at respected research institutions to find medicines that can slow the aging process. Many of the compounds under study show promise in mice and even humans, and some are in clinical trials.
Better health in old age is not just about individual benefits. By 2030, 73 million baby boomers in the United States will be 65 or older. By the same year, experts project, there will be a billion people 65 and older globally. And though people are living longer, they are not necessarily living healthier than previous generations.
An aging population
Estimates suggest there will be a billion people age 65 and older globally by the year 2030, and the global figure could hit 2.5 billion by the end of the century.
World population by age group
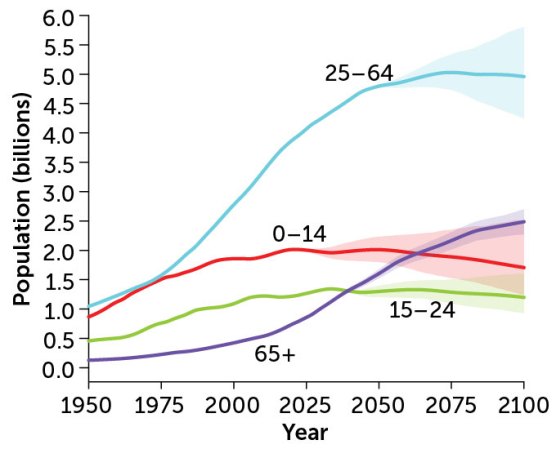
“There’s this fear of what is this going to do to our health care system,” says Laura Niedernhofer, a geneticist and researcher studying aging at the University of Minnesota in Minneapolis. “And it goes well beyond just health care. We don’t have the nursing homes. We don’t have the personal care staff to deal with this at all.” Drugs to help keep older adults healthy, active and independent would be a societal boon.
But whether developing such drugs is even possible remains to be seen. Getting the medicines to market means securing more funding, overcoming stumbling blocks related to study design and combating near constant hype.
How did geroscience begin?
The advent of modern medicine and public health has more than doubled the average human life span — from about 30 in the early 1800s to more than 70 today. “This is perhaps one of the biggest things that has happened to humankind, period,” says Jamie Justice, a geroscientist who heads the health domain at the XPRIZE Foundation, which holds competitions to spur technological developments and announced a new prize related to aging in November. “We are a lot less dead than we used to be because of where public health and modern medicine has gotten us.”
There’s a downside, of course. We’re living long enough to see the frailty and illness that comes with old age. Cells stop dividing, DNA degrades, the immune system falters. We become increasingly vulnerable to disease. Many of us spend our last decades beset by medical maladies — broken bones, weakness, dementia, cancer, heart disease and more. Doctors can do little more than play whack-a-mole, beating back illnesses one at a time.
For decades, scientists thought the gradual decline that comes with old age was unavoidable. But experiments in the 1980s and ’90s suggested that the process might not be so fixed.
In one notable experiment, Cynthia Kenyon, a molecular biologist at the University of California, San Francisco, and colleagues found that mutations in a single gene in the roundworm C. elegans could double its life span. Typical 13-day-old worms barely moved. “The animal is clearly in the nursing home,” Kenyon said in a 2011 TED Talk. The mutant worms moved as if they were much younger, and they lived longer too.
For researchers interested in human health, this and similar findings from other teams led to a profound realization: Perhaps the aging process is malleable. If so, scientists might be able to develop therapies to attack the root of aging rather than simply combating the pileup of diseases.
By the late 2000s, “the whole perspective of the scientific community changed,” says Felipe Sierra, who was then a program officer at the National Institute on Aging in Bethesda, Md. Aging biology moved from a phase of description into a phase of molecular investigation. Sierra wanted a name to bring the field together. He landed on geroscience, a word he had first seen in a grant proposal by another researcher studying aging, Gordon Lithgow. “Gero-” comes from the Greek word for old man. It wasn’t difficult to convince other researchers to get on board. “Everybody listened to me because I was in charge of the money,” says Sierra, now chief scientific officer at Hevolution Foundation, a nonprofit that funds geroscience research.
What compounds might fight aging?
Though there are no proven therapies for people yet, geroscientists are eyeing several compounds that can slow the aging process, at least in worms, fruit flies and mice. Some have already been tested in humans, and many more clinical trials are under way. Which will work? “Let me see. Let me look at the crystal ball,” Sierra jokes. “Who knows?”
Perhaps the best studied is rapamycin, a compound first discovered in a soil sample collected in 1964 from Rapa Nui, or Easter Island. Today, people who receive organ transplants take the drug to help keep their immune systems from rejecting the foreign tissue. But rapamycin also prolongs life in yeast, flies and mice. And it’s being tested in people in clinical trials. How it counters aging isn’t entirely clear. The drug inhibits a protein complex called mechanistic target of rapamycin, mTOR for short, which plays a role in cell growth and protein synthesis. This inhibition appears to have wide-ranging effects, including reducing inflammation, clearing old and damaged cells, and altering cellular metabolism — some of the key processes that researchers think are to blame for the aging process.
Rapamycin isn’t the only drug to impact mTOR. Researchers at the biotech company resTORbio tested other mTOR inhibitors in elderly adults to try and improve immune function. About 250 people participated in the clinical trial, which tested two mTOR inhibitors alone and in combination compared with a placebo. In 2018, the team reported that those who received the drugs had fewer infections and mounted a better response to the flu vaccine. The company tried one of those compounds in a subsequent study, though, and it failed to show an effect on self-reported respiratory illnesses. resTORbio no longer exists, but the company’s chief medical officer, Joan Mannick, hasn’t given up on mTOR inhibitors. She cofounded a new company called Tornado Therapeutics, based in New York City, that is working to develop new rapamycin analogs, or “rapalogs.”
Another promising class of drugs targets cells that have stopped dividing but don’t die. These senescent cells release chemical signals that can trigger inflammation, disrupt tissue repair and harm neighboring cells. In some cases, these signals even prod neighbors to become senescent too.
The drugs, called senolytics, aim to eliminate senescent cells by prompting them to commit suicide. After showing promising results in mice, senolytics are now being tested in humans. More than 25 clinical trials have either been completed or are under way.
One of the most commonly tested senolytic regimens is a combination of two compounds: the anticancer drug dasatinib and quercetin, an antioxidant that occurs naturally in grapes, berries and other fruits and vegetables. Other research efforts plan to compare fisetin, a compound found in strawberries and apples, with a placebo to see if it has an impact on frailty and markers of inflammation in the blood.
Unity Biotechnology, based in San Francisco, is focused on senolytic therapies exclusively. The company’s most advanced compound, called UBX1325, targets a protein abundant in the blood vessels and retina that regulates cell death. Preliminary results from a trial in patients with diabetic macular edema, a thickening of the retina related to diabetes, suggest that the compound can improve eyesight.
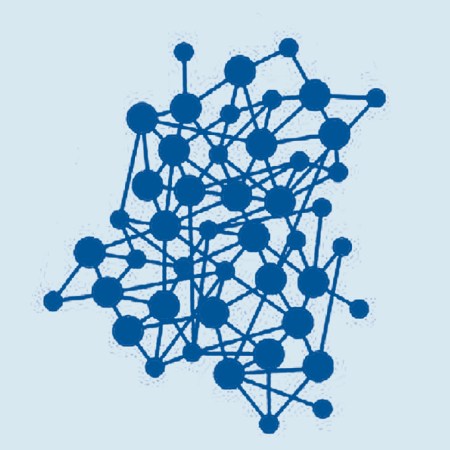
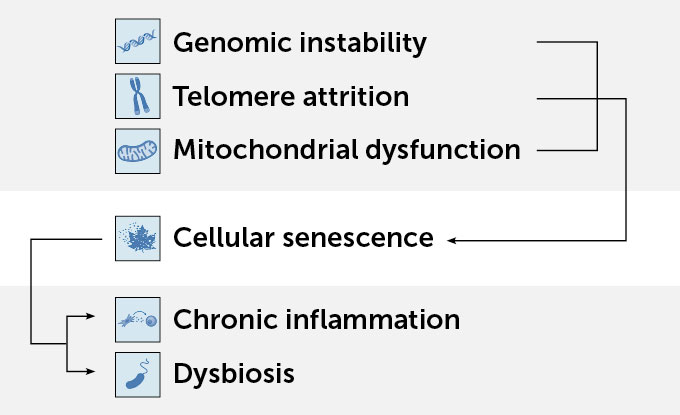
12 hallmarks of aging
Researchers have identified a dozen hallmarks of aging that appear capable of nudging life span — and likely health span — one way or another across a range of animals. A network of interactions among genes and their products underlies these interconnected hallmarks, and it’s that network that drugs such as rapamycin and senolytics are targeting.
Genomic instability includes changes to DNA, chromosomal rearrangements and defects in nuclear architecture.
Telomere attrition is the cumulative damage or loss of DNA at the ends of chromosomes, called telomeres.
Epigenetic alterations can change how a gene is expressed without changing the DNA itself, such as methylation.
Loss of proteostasis refers to imbalances in proteins in the body, which can lead to the formation of protein aggregates, as in Alzheimer’s.
Disabled macroautophagy leaves cells unable to sequester and digest material in the cytoplasm, thus affecting the replacement of organelles.
Dysbiosis is the disruption of the body’s microbial communities, which play a role in nutrient digestion, disease protection and more.

Chronic inflammation increases with aging, both across the body and locally, and typically comes with a decline in immune function.
Altered intercellular communication brings more noise into the system, disrupting neural, neuroendocrine and hormonal signaling.
Stem cell exhaustion leads to a reduction in tissue renewal rates across the body and can limit tissue repair after injury.

Cellular senescence, when cells stop dividing but don’t die, has been linked to kidney disease, diabetes, Alzheimer’s, Parkinson’s and more.

Mitochondrial dysfunction can prevent a cell from producing the energy it needs, as well as contribute to inflammation and cell death.
Deregulated nutrient-sensing affects a whole series of pathways that shape cell activity, which makes diet a practical aging intervention.
Diet is also known to profoundly affect the aging process. Studies have found that the low-carb ketogenic diet, for example, can help mice live longer. But restrictive diets can be hard to follow and have side effects. Broadbent followed the ketogenic diet for a month or so, but his cholesterol levels went dramatically up. Ketone ester, the compound Broadbent might be downing each morning for the Buck Institute’s clinical trial, may mimic the longevity benefits of such diets.
When the body runs out of glucose to use for energy, the liver creates another source by converting fat into molecules called ketone bodies. “If we don’t eat for a day or so, we’ll start to make ketone bodies,” says John Newman, a geriatrician at the Buck Institute who is leading the trial. “And we’ll make more and more the longer that we starve in order to fuel our bodies.” These compounds are more than just fuel. They help regulate inflammation and control other cellular processes, many of them involved in the aging process. Drinking ketone esters, which quickly break down, is a way to deliver the ketone bodies without the diet.
Among the dozens of clinical trials testing potential gerotherapies, very few are yet assessing their ability to prevent the onslaught of diseases that come with aging. Instead, the goal is establishing safety or seeing whether a compound can nudge some biomarker in the right direction. And many of the potential treatments under study are natural compounds or existing drugs that are already off patent, which might leave drug companies hesitant to invest in future trials or to seek approval from the U.S. Food and Drug Administration or other regulatory agencies.
What’s more, as James Kirkland, a geriatrician at the Mayo Clinic in Rochester, Minn., points out, many of the clinical trials happening now will fail. “In fact, most will,” he says. That’s just a part of drug development.
For now, some companies are bolstering their chances of success by pursuing many options. Cambrian Bio, the parent company of Tornado Therapeutics, for example, is “taking a number of different shots on goal,” Peyer says. “We don’t know which drug is going to really be the first multidisease preventative.”
Aging hallmarks link up
In one example of interconnections, several hallmarks can affect cellular senescence, which then drives inflammation and dysbiosis.
What are the barriers to progress?
One of the big challenges for geroscience is to figure out how to show that a compound prevents age-related diseases in people. Scientists would have to give the drug to healthy people and then track their health as they age, an expensive and time-consuming endeavor. “In mice, it takes us four years. In humans, it would take decades and tens of thousands of people,” Niedernhofer says.
An easier path to the clinic would be to develop these therapies as a treatment for a single disease rather than a multidisease preventive. “That’s something that the FDA is very comfortable with,” says Nathan LeBrasseur, a researcher studying aging at the Mayo Clinic. Once the drug is approved for one indication, it would be much easier to seek approval for others — and potentially widen to a preventive. “The absolute irony of all of this is, to try and advance geroscience, we’re going right back to the old way of doing things, which is one disease at a time,” Niedernhofer says. For example, Unity is developing its lead antiaging candidates as therapies for a variety of eye diseases.
One group of researchers, however, has developed a clever work-around. Rather than treating healthy people and waiting for them to age, the team has devised a study that will recruit people who have one age-related disease and assess whether a drug reduces the time it takes to develop another. In this case, the researchers have chosen the diabetes drug metformin. Metformin has a long safety record, and studies suggest it can impact heart disease, cancer and cognitive decline. Metformin may even reduce the risk of long COVID. The precise mechanisms that underpin these effects aren’t entirely clear. The study, called Targeting Aging with Metformin, or TAME, will look at things such as cardiovascular events, cancer, cognitive decline, dementia and death.
But nearly eight years after investigators first announced the 3,000-person trial, they’re still trying to get together funding. Metformin is cheap and readily available, no longer protected by a patent, so drug companies have no incentive to develop it for aging. Nir Barzilai, director of the Institute for Aging Research at the Albert Einstein College of Medicine in New York City, who is leading the study, has started telling people the trial will start in January. “And as long as I don’t say which year, it will be true,” he jokes.
Part of what holds the field back is society’s approach to medicine, says Justice, of the XPRIZE Foundation. “We have a model of medicine that prioritizes treatment of diseases,” she says. “You get one disease. You treat one disease. You restore homeostasis.” But that approach isn’t relevant for aging. Geroscientists also have to fight society’s views of aging. The mind-set is “things get old. It just happens. There’s nothing you can do, just let it go,” Justice says. “I think that is actually a fundamentally ageist view, as if people who are older don’t have a right to health.”
Geroscientist Matt Kaeberlein of the University of Washington in Seattle agrees. No one would argue that we shouldn’t develop therapies for Alzheimer’s or cancer because these diseases are a natural part of getting older. So, he asks, why would this argument hold for aging? “I don’t really see what the field is trying to do as any different than trying to cure disease,” he says. “It’s just a much more efficient and effective approach, or it’s likely to be.”
Kaeberlein thinks dogs, because they age much faster than people, could bridge the gap between lab studies in mice and therapy approval. “You can do longevity clinical trials in dogs that you can’t do in people,” he says. And companion animal medications are regulated much like human medications. The Dog Aging Project, which Kaeberlein codirects, is testing rapamycin in 500 middle-aged dogs to assess its impact on the heart, the immune system, cancer incidence and cognition.

But even if geroscientists find compounds that treat the decline that comes with aging, it’s not clear whether they will compress the period of age-related illness — that’s the goal — or simply delay it. It’s also uncertain whether such therapies might add to the average life span and, if so, how many years. John Davis, an ethicist at California State University, Fullerton, worries about how such increases might affect demographics. If the average life span jumps to 120 years, the effects aren’t too pronounced, he says. If it goes far longer, there is the potential for “really spectacular increases in population on a planet that I personally feel is already overloaded.” And then there are concerns about how longer life might impact existing inequalities. “Billionaires who live longer have more time to accumulate even more wealth,” Davis adds.
Beware the antiaging hype
There’s another potential obstacle: hype.
No one can say with any certainty that there will be a pill to prevent aging. Yet that hasn’t stopped some companies and less scrupulous researchers from cashing in. The public’s interest in escaping aging makes overselling results enticing. In 2019, for example, the FDA warned consumers against receiving infusions of plasma from young donors, which some companies offered for $8,000 a liter. The treatment was based on promising mouse studies that gave older mice blood from younger mice, either via transfusions or by connecting the two animals’ circulatory systems. The young blood appeared to rejuvenate the older animals’ muscles, livers and brains, but the benefits haven’t been proved in human patients.
The internet is likewise rife with supplements and even prescription medications with purported antiaging benefits. Many of the pills being touted as age-reversing miracle drugs are the same compounds geroscientists are currently testing in trials. “[Companies] start trying to sell it to the public before it’s been tested for safety and efficacy,” Olshansky says. That can make it especially difficult for consumers trying to sort fiction from fact.
LeBrasseur is concerned that if scientists oversell their progress, they run the risk of losing public trust. And a rush to clinical trials might lead to safety problems. “If something bad happens, that’s going to set the entire field back,” he says. “I just think we have to be patient and humble.”
A student of Newman’s, at the Buck Institute, asked him recently how geroscience has changed clinical practice. “The honest answer is it hasn’t at all,” he says. “We’re still building the data. We’re still running the clinical trials waiting for it to come in. And this all takes time.”
But Broadbent, and many others, aren’t satisfied waiting for settled science. He likes to do his own research, and ketone ester seems like a good bet. The particular product he may be drinking as part of the clinical trial is now being sold as a supplement, and he plans to continue taking it after the trial ends. “I’ll sign up right away,” he says. “I’ll be on an annual subscription.”
Many scientists are convinced that the geroscience revolution is coming. Until then, there’s a tried-and-true method for improving your health span. It’s the advice any doctor will give you: Eat a balanced diet, exercise, get vaccinated and avoid tobacco and alcohol.







