How a deadly fungus is so good at sticking to skin and other surfaces
Unlike other fungi, Candida auris uses electrical charges to glom onto things
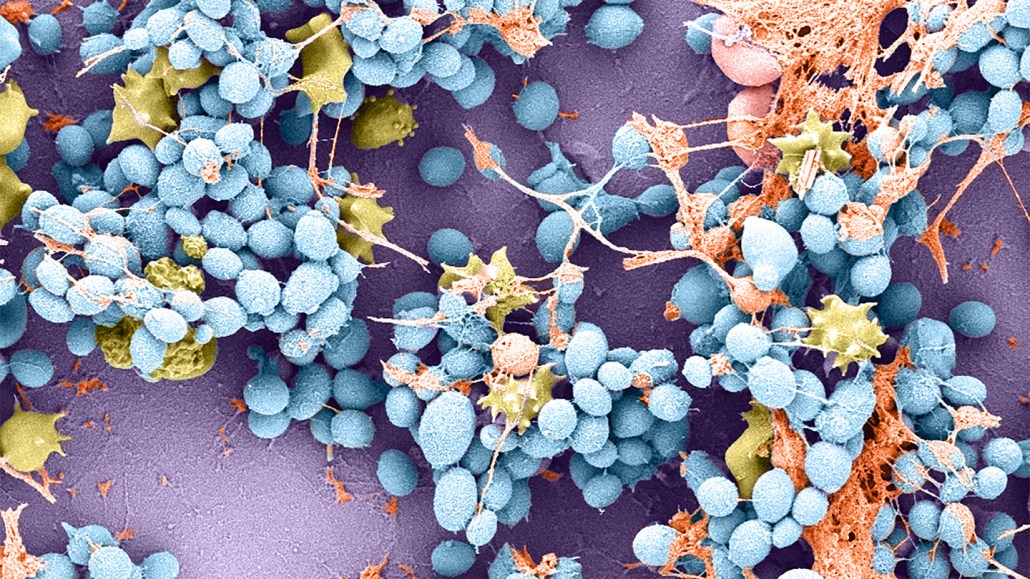
Candida auris (blue, shown magnified 5,000 times) has developed a barnacle-like method for sticking to surfaces. This electron micrograph shows the fungus sticking to a catheter used in a rat. Immune cells are shown in yellow.
Robert Zarnowski