Gravely damaged brains have ‘bottleneck’
Signaling loop in healthier subjects is broken for patients in vegetative state
Talk between the brain’s decision-making center, or frontal cortex, and other brain regions might distinguish aware individuals from those stripped of conscious thought. Identifying such signaling malfunctions could speed the diagnosis of vegetative states and give scientists insight into such devastating disorders, an international team of researchers reports May 12 in Science.
Today, diagnosing a vegetative brain is an uncertain enterprise, says John Whyte, director of the Moss Rehabilitation Research Institute in Elkins Park, Pa. Patients classified as vegetative can’t act in any purposeful way under any observable circumstances. Patients deemed minimally conscious, however, show some capacity to understand and interact with the world — for instance, by moving a finger on command. Distinguishing between the two can take weeks of behavioral testing, and misdiagnoses are common.
With better diagnostics in mind, Mélanie Boly of the University of Liège in Belgium and colleagues monitored the brain responses of 22 healthy volunteers, 13 patients previously diagnosed as minimally conscious and eight diagnosed as vegetative to fluctuating blips of sound. Minimally conscious and healthy subjects responded to a surprising change in the pitch of the sounds with bursts of brain activity about 170 milliseconds long. Responses from vegetative patients lasted less than 100 milliseconds.
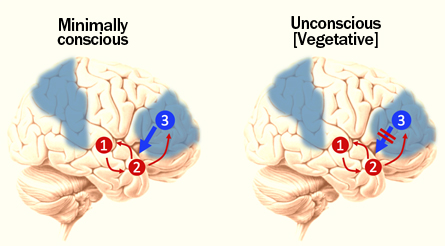
Using statistical tools, the researchers filtered through a number of possible causes of such shortened brain activity before determining the most likely culprit. The team concluded that damage to communication paths within the brain, not just to individual regions like the frontal cortex, seemed to typify the vegetative state. When healthy or minimally conscious brains registered unexpected noises, electrical signals passed from the brain’s auditory centers to the frontal cortex, which signaled back in a long-lasting loop. In vegetative patients, however, the loop screeched to a halt. Signals could get into the frontal cortex, but neurons there couldn’t send messages back. “The bottleneck, if you will, is the top-down connection,” says Boly.
Whether such electrical brain patterns could make useful diagnostic targets depends on several big uncertainties, Whyte says. For instance: “Are the types of patterns seen in this study stable hour to hour, day to day?” he asks.
A more important question may be what such connections can tell scientists about the brain and, by extension, brain damage. According to one theory, the frontal cortex learns to expect certain things — patterns of sound, for instance — and communicates those expectations to the rest of the brain. When those expectations aren’t met — the tone changes, perhaps — the brain has to think on its feet, interpreting surprising information, says study coauthor Karl Friston, a researcher at University College London in England. But vegetative patients can’t communicate their predictions and, therefore, the information coming into their brains may just be that: information. “In order to act and respond adaptively,” Friston says, “you clearly have to have some representation of the causal structure of what is happening in the world.”