Serotonin: What the gut feeds the bones
Chemical messenger plays a surprising role in determining the strength of the skeleton
The hip bone is connected to the backbone. The backbone is connected to the neck bone. And lately, scientists have begun to think that all dem bones may be connected to the intestine — at least by biochemical signals. If the current evidence holds up, it means that a chemical better known for influencing the brain may also corrode the internal structure of the skeleton.
Such is the state of research into bone biology: “The more we understand, the more complex it gets,” says Clifford Rosen of the Maine Medical Center Research Institute in Scarborough. Rosen is one of a growing number of researchers who think that the brain, intestine and skeleton are conducting an ongoing biochemical negotiation that affects the ebb and flow of tissue building inside bones. One of the chief currencies appears to be serotonin, a neurotransmitter most famous for its role in depression.
The idea that serotonin might be bad news for bones came as a surprise almost a decade ago. And the notion that the intestine hosts a serotonin-bone command center — first described last fall — was more surprising still. “It’s thrown the field into a bit of an uproar,” says Michael Bliziotes of Oregon Health & Science University in Portland.
By eavesdropping on the crosstalk between the intestine and skeleton, researchers hope to find much-needed ways to help protect bones into old age. More than 300,000 elderly Americans suffer hip fractures each year; one in five die within a year from complications of the injury. Bone-strengthening medications have been hard to come by, largely because bone is simultaneously one of the most simple and most convoluted structures in the body — brilliant and straightforward in engineering, yet owing its construction to an elaborate relationship with internal organs.
It’s easy to perceive bones as dense and dead. But on the inside, bones are not hard like blocks of wood, but airy, like sponges. The internal, honeycomb-like scaffolding allows bones to be sturdy without leaving them too heavy. Strength isn’t determined by density but by the makeup of the matrix within (in the same way a china plate is denser than a plastic one but less likely to survive a drop on the floor).
Neither are bones dead. Throughout life, bones are constantly remodeling themselves, constructing new tissue in some places, clearing out old bone in others. As with hair or skin, worn bone
tissue is constantly replaced with new in what is called bone turnover. Bones generally reach their maximum strength in early adulthood, after which they gradually wear away. After decades of erosion, bone density sometimes dips low enough to qualify as osteoporosis. That disorder occurs largely because, as people age, cells that secrete new bone, called osteoblasts, don’t work as robustly as osteoclasts, cells that resorb or break down bone, especially in postmenopausal women. Most treatments for osteoporosis slow the loss of bone; the one drug that can build bone costs thousands of dollars a year per patient and isn’t prescribed as a long-term option.
Nutrients and hormones — including vitamin D, calcium and estrogen — are crucial to maintaining a favorable rate of bone turnover. Strength training also tips the balance toward osteoblasts. These aspects of bone biology are clear. But scientists acknowledge that much of the skeleton-building story remains a mystery.
Unexpected connections
The link between serotonin and bones turned up, as scientific discoveries often do, when researchers were looking for something else altogether. In 2000, scientists at Duke University in Durham, N.C., were conducting studies on substance abuse with mice specifically bred to lack certain brain molecules called dopamine transporters, which interact with the neurotransmitter dopamine. The scientists noticed that the mice seemed to have extraordinarily brittle bones. Bliziotes, an endocrinologist who had been collaborating with the Duke team, began to search for a biochemical explanation.
Although they went searching for dopamine transporters in the bones of normal mice, the researchers were astonished to instead find transporter molecules for serotonin, Bliziotes and his colleagues reported in the journal Bone in 2001. And the serotonin transporter molecules turned up in all types of bone cells —osteoblasts, osteoclasts and, later work showed, osteocytes, cells derived from osteoblasts. That same year, a Dutch research team studying chicken embryos also discovered a role for the neurotransmitter in bone. “Before 2001, it wasn’t known that serotonin had any involvement in bone,” Bliziotes says.
In the brain, low levels of available serotonin are thought to contribute to depression. Indeed, the most famous antidepressant in the medicine cabinet — Prozac — works to boost the supply of serotonin available in brain synapses, junctures where neurons communicate. So what was serotonin doing in bones?
Apparently, making them weaker: Serotonin seems to interfere with the production of the bone-forming osteoblasts. Following the discovery of a serotonin connection to bones, Bliziotes and others began to worry about the more than 8 percent of U.S. adults who take Prozac and related drugs called selective serotonin reuptake inhibitors, or SSRIs, to amplify serotonin. In 2007 in the Archives of Internal Medicine, Bliziotes and his colleagues described a study of almost 6,000 older men involved in an osteoporosis investigation. Men taking SSRIs had lower average bone density than those not on the drugs. A related study of postmenopausal women found that bone density declined in those taking SSRIs twice as fast as it did in other women.
“I think the major question right now is — if depressed people are going to be treated with SSRIs, are we subjecting them to risk of fracture?” says Bliziotes. The issue is still under investigation, largely because the studies are difficult to interpret. Among people taking SSRIs, Bliziotes says, “most of them are going to have been put on SSRIs for symptoms of depression. Depression alone has been associated with lower bone density.” And people with depression may have weaker bones not from their own physiology but because of lifestyle changes that can accompany the condition, including poor nutrition and low levels of exercise. “We haven’t done randomized trials,” Bliziotes notes.
To further investigate the role of serotonin, researchers have looked to bone tissue itself to characterize the neurotransmitter’s influence over bone cells. These studies have led to a family of proteins called Wnt. (The name comes from a combination of two genes first discovered in fruit flies — wingless and INT — and is pronounced “wint.”) Wnt proteins have so many functions that a book about them takes up two volumes. Medical researchers have an intense interest in Wnts because the molecules appear to be involved in cancer, heart disease, obesity and many other conditions. But Wnts also orchestrate basic development and maintenance of body parts.
The fruit fly Wnt proteins have human counterparts, including, of special interest to bone researchers, the signaling protein Lrp5. About a decade ago, researchers found that mice with a mutated form of the gene for Lrp5 had low bone density. In people, mutations in this gene can lead to two distinct effects on bone. One is osteoporosis-pseudoglioma, a rare syndrome that affects children, giving them bones often too fragile even for walking, along with vision problems early in life. A different mutation in the gene produces a condition at the other end of the clinical spectrum: high bone mass syndrome, rendering bones unusually dense and protected against osteoporosis. Looking at the effects of these mutations in people, it became clear that Lrp5 had the power to make or break bone.
“Since the discovery of Lrp5, there has been a tremendous effort to study how it works,” says Gerard Karsenty of Columbia University Medical Center. Until last year, most researchers assumed that whatever the role of Lrp5, its importance started and ended in the skeleton. Then in November, Karsenty and his colleagues published a paper in Cell that was, in bone research circles, jaw dropping: In experiments with mice, he demonstrated that Lrp5 affects the production of serotonin in the duodenum, the segment of the small intestine where most digestion of food occurs (SN Online: 11/26/08).
Despite the neurotransmitter’s fame in the brain, 95 percent of the body’s serotonin is made in the intestine, from the amino acid tryptophan, which is a component of dietary protein (and lore aside, is no more prevalent in turkey than other meats). After a meal, the intestine turns tryptophan into serotonin, while platelets from the bloodstream ferry serotonin throughout the body. It’s an entirely separate circuitry from serotonin production in the brain. Serotonin made in the brain stays in the brain, and the two different sources don’t mingle.
Karsenty’s experiments found that Lrp5 interferes with the production of serotonin in the gut. To arrive at this conclusion, he and his colleagues bred mice with gene mutations known to hamper bone formation. Yet when bone cells from these mice were isolated in laboratory dishes, and thus removed from exposure to serotonin, they grew normally. In short, when not exposed to serotonin, the tissue appeared to be just fine. Similarly, when normal bone cells were exposed to serotonin in the laboratory, their growth slowed. According to these experiments, the problem with bone growth seemed to lie outside of bone cells and not in some faulty bone-building mechanism.
That led Karsenty’s team to search for other organs that might affect bone formation. In the Cell paper, he and his colleagues reported that Lrp5 acted in the gut, blocking a key enzyme necessary for the conversion of tryptophan to serotonin. When the intestine is awash in Lrp5, less serotonin gets produced, and bones remain stronger. Less Lrp5 means more serotonin, and weaker bones. “This study uncovers an unanticipated molecular mechanism accounting for the Lrp5 regulation of bone formation,” the researchers wrote.
Serotonin’s long reach
Key questions remain. Among them: How might all this knowledge one day translate into a medical benefit? Other, broader issues go beyond the skeleton. Serotonin isn’t present just in the brain, intestine and bones. It works throughout the body, tweaking many different systems, including the cardiovascular system and digestion. “If you turn off the main site of synthesis, what kind of bad effects are you going to have?” says Bliziotes. No one can be sure until the cellular machinery is better understood.
Rosen also wonders how the brain comes into this picture. Although the serotonin in the brain and intestine never meet, evidence suggests that the brain may have other effects on bones. Some of that influence may even act through the digestive system. The hormone leptin suppresses appetite but is also implicated in the regulation of bone mass. And Rosen points to other hints of a brain-bone connection. For example, the rate of new bone formation increases after traumatic head injury.
Rosen isn’t surprised that the skeleton would have a connection to the gut. Bones are the body’s biggest storehouse for calcium. Bone turnover slows after eating, probably to keep calcium locked in the bones, he says, and increases during fasting. Through serotonin, the intestine may be cueing bones to slow or to rev up turnover based on the body’s need for calcium. Ultimately, he believes, scientists may find that bones have a more intimate connection to other organs than anyone first thought. “I think we have just scratched the surface,” Rosen says.
For now, scientists are eager to learn more about serotonin and how critical a role it may have in bone structure. More than anything, says researcher Fanxin Long of Washington University Medical School in St. Louis, the new findings are a stark reminder that no organ in the body operates as its own, isolated fiefdom. “It highlights a picture that has become more and more clear,” Long says. “Different organs in the body talk to each other.” In a language scientists hope to one day fully understand.
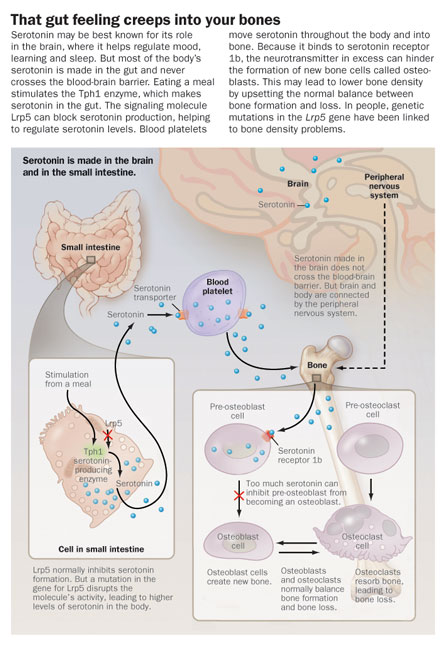
That gut feeling creeps into your bones
Serotonin may be best known for its role in the brain, where it helps regulate mood, learning and sleep. But most of the body’s serotonin is made in the gut and never crosses the blood-brain barrier. Eating a meal stimulates the Tph1 enzyme, which makes serotonin in the gut. The signaling molecule Lrp5 can block serotonin production, helping to regulate serotonin levels. Blood platelets move serotonin throughout the body and into bone. Because it binds to serotonin receptor 1b, the neurotransmitter in excess can hinder the formation of new bone cells called osteoblasts. This may lead to lower bone density by upsetting the normal balance between bone formation and loss. In people, genetic mutations in the Lrp5 gene have been linked to bone density problems.
Laura Beil is a freelance science writer in Cedar Hill, Texas.