What’s it like to live with deep brain stimulation for depression?
Learning to live with the treatment comes with physical and emotional challenges
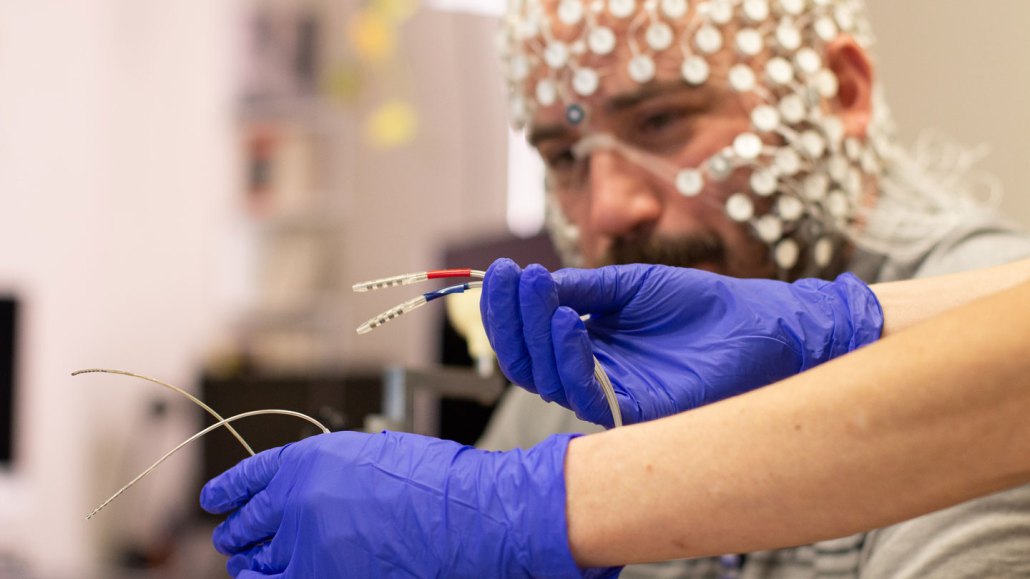
External electrodes on a cap measure Jon Nelson’s neural signals as part of a research project to see how the brain changes with DBS.
AIDAN KAHN

Electricity Saved My Brain
This is the fourth part in a series on deep brain stimulation for depression. Read from the beginning.
[Content note: This story contains discussion of suicide.]
“The only thing I’ll slightly complain about — and it’s very vain — I only wish the batteries in your chest didn’t show up so much,” says Patient 001.
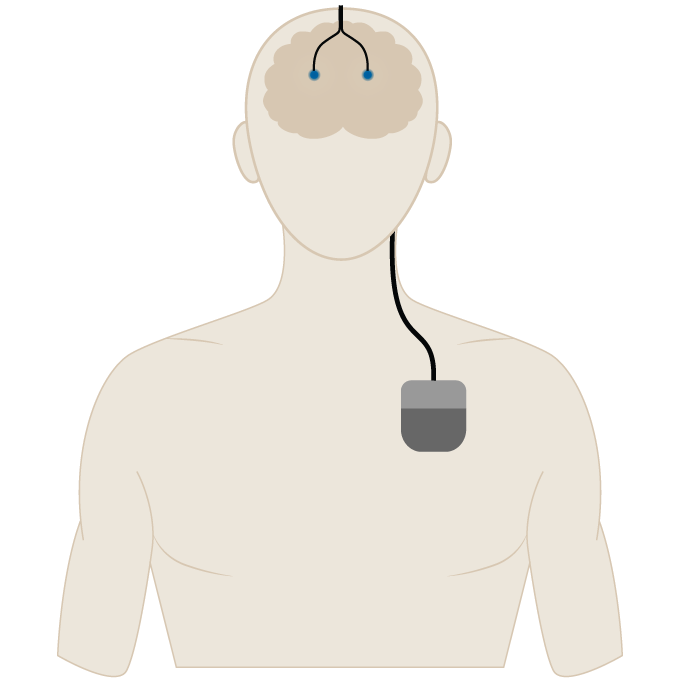
There is an intense physicality to deep brain stimulation for depression. Participants have two slight bumps on their head, wires under the skin of their neck and a battery-powered control unit implanted under the skin in their chest.
Because he was implanted with two sets of electrodes, Patient 001 has two battery packs, one on each side of his upper chest. He lives in a hot place near the ocean. “It just sucks I can’t take my shirt off at the beach and not be self-conscious about that.” Sometimes the devices in his chest feel alien to him when he’s going to sleep. “I put my hand on it to be comfortable,” he says.
Amanda has a strained relationship with the device, too. “I don’t like the idea of it. I don’t like how it feels. Every time I accidentally touch the wire in my neck, I’m like, ‘Ugh, ugh, I don’t like it,’” she says. “It’s getting better, but sometimes I can still feel that thing in my chest just sitting there.”
She also points out the annoyingly low-tech charging process, which is done with a wireless charger draped around her neck. Her charger shows only 10 percent increments, and the screen is on for only a minute before it locks up, without indicating that the charging is done. “They can get better at that part,” she says.
In addition to the charging, there are lots of tasks these volunteers complete as part of the research — surveys, mood ratings, video journals. Twice daily, Amanda clicks what looks like a TV remote at home to collect brain data. “I’m Bluetooth-enabled,” she says with a laugh. “I upload from the computer to the server at the hospital.” She and others also make regular trips to the lab at Mount Sinai.
These days, Jon takes the train from his house just outside Philadelphia to Mount Sinai so often that he knows exactly which crack in the sidewalk to stand by as he waits for his train at the New Jersey Transit station. On one of his visits to the lab, a mess of scalp electrodes were eavesdropping on his brain. The scientist doing the measurements, neuroscientist Allison Waters, mentioned that his electrode leads were zipping 130 pulses of electricity into his brain per second.
“She just said it off the cuff,” Jon says. Later, with his daughter, Jon did the math for a full day, doubling it for each side: “22 million, 500 thousand electrical pulses to my brain,” Jon says. “That’s what has kept me alive.”
During Jon’s surgery on August 22, 2022, doctors told him that his only job was to be present. After his incisions healed, he was given a new task: rehabbing his brain. Jon was initially dismissive of the new job. He already felt fantastic, cocky almost, and didn’t buy that he needed to work hard on rehab. “In the back of my head, I’m like, ‘OK, weirdos. I’m not sick. This is great. I’m good. I got this.’”
But about six weeks after his surgery, everything fell apart.
A malaise crept in, and Jon freaked out. “Oh my God, I feel it,” he said. “I feel it in my body.” He snapped right back into the habits that depression solidified: overeating, sleeping too much and hiding away from his family. “My wife, I’ll never forget it, was like, ‘Hey, we got an appointment at the school.’” But Jon told her he couldn’t make it; he was busy. It was a lie. “I didn’t have anything going on,” he says.
Jon knew that as part of the study protocol, around the sixth month, researchers would turn off his stimulation, a looming event that made him intensely anxious. His shift alarmed him so much that on the night of October 6, he sent an email to the Mount Sinai psychiatrist Martijn Figee to ask if his stimulation had been turned off earlier than planned. “Is there an earlier part of the program where it gets shut off too, such as now, and that is also part of the experiment?” Jon wrote. “Even if it was shut off, could you even tell me that?”
An hour and a half later, the email back was clear: “Your device is absolutely on.” His psychologist would address it with him at their next appointment.
Relearning to live with emotions
As brain implants are used more and more, the risks of DBS have become somewhat clear. Regardless of why a person is getting it or where in the brain it targets,the technique can, like any medical procedure, go sideways. Electrode leads in the brain can break; the chest controller can fail; batteries can die. Infections, in both the head and chest, are a risk, as is wire tethering, a painful condition, also called bowstringing, in which scar tissue grows around the wire in the neck.
DBS can also carry risks that are distinct from other surgeries. Electrical stimulation in certain parts of the brain has been linked to unwanted behavioral changes. For people receiving stimulation for Parkinson’s disease, there have been cases of gambling problems and hypersexual behavior.
In one unusual case, a Dutch man treated for obsessive-compulsive disorder developed a brand-new and intense affinity for Johnny Cash hits, especially “Ring of Fire,” “Folsom Prison Blues” and “Sunday Morning Coming Down.” When his stimulations diminish or his batteries die, the man subconsciously switches back to listening to his old favorites — Dutch-language songs and classics by the Beatles and the Rolling Stones.
People being treated with DBS for depression have experienced relapses when the device accidentally stops working, for instance due to a battery failure or a wire breaking. But that’s not what happened to Jon.
Worries over spiraling dark moods surface among people with DBS for depression, says psychologist Shannon O’Neill, who works with Jon and other people treated with DBS at Mount Sinai. “We often talk significantly about the difference for them of how they can distinguish between depression and normal everyday sadness,” O’Neill says. This is the rehab part, she says. People who have lived with severe depression for years need to relearn how to recognize and tolerate garden-variety emotions, including sorrow.
As O’Neill describes ordinary sadness, it reminds me of the analogy that emotions are like the weather. We can spend the morning under heavy cloud cover, and then maybe we luck out with a full-blast sunny afternoon. But it’s fleeting. Likewise, our feelings are impermanent, O’Neill says. “Negative emotions come and go, just like positive emotions come and go. It can be passing and not ever-present.”
Emily Hollenbeck, whose DBS surgery was in 2021, says her recovery took time. “You’re letting your brain relearn how to live in the world without the constant threat of severe negativity, suicidality, all of that.” She had to learn how to cope with emotions, and trust that she’ll get through bad situations. “Basically, I’m relearning how to ride the bike, you know?”
Understanding that these feelings are transitory — that ups and downs happen — is something people with severe depression haven’t practiced, because they hadn’t had to. They’ve been perpetually stuck under heavy cloud cover. Emerging into an emotional landscape with those ups and downs can be intensely unsettling.
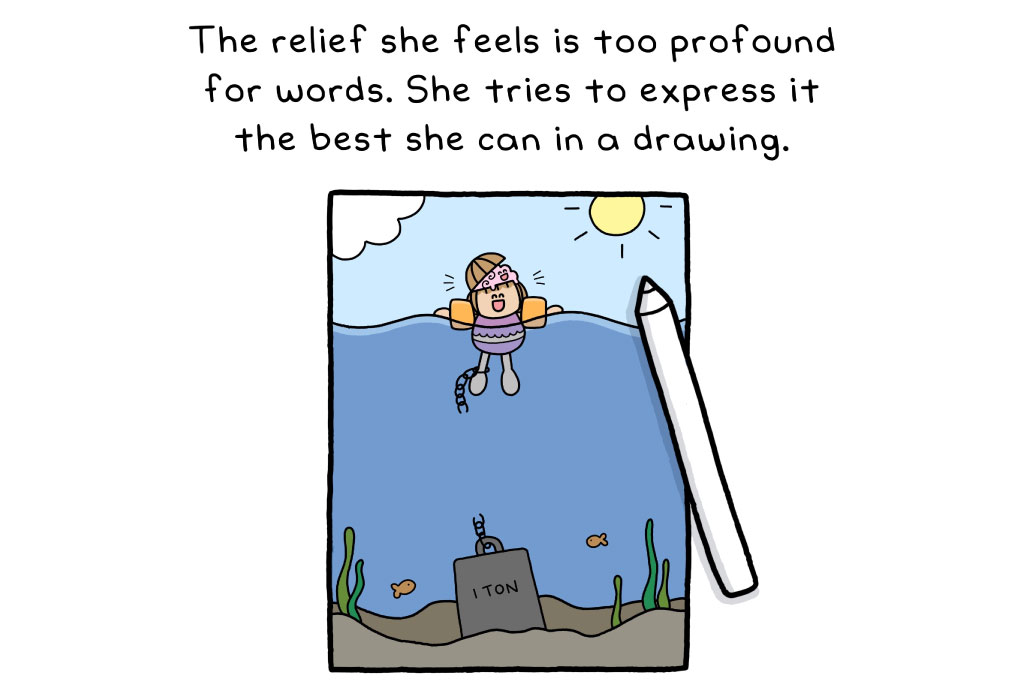
“At first it was scary,” says Amanda, who had DBS surgery last fall. “At first I felt like I was standing on the edge of a cliff.” An artist, Amanda draws her experiences to help her think them through. One of her pictures shows a cartoon Amanda wearing a rainbow shirt, standing high on a ledge of bright green grass with blue sky overhead. But she’s looking over the edge to the darkness below. “I had been pulled out of this giant pit, and I was worried that I would fall back in it again.”
But she hasn’t. When people recover from depression with DBS, they generally stay well, several studies suggest. Between three and six years after surgery, about 60 percent of patients had sustained improvements, Mayberg and colleagues reported in 2011 in the American Journal of Psychiatry. In a longer-term study, most of a group of 28 people who had deep brain stimulation for major depression or a type of bipolar disorder saw benefits for more than eight years, the researchers reported in 2019 in the same journal.
Does DBS make people happy?
The idea of a machine forcing happiness on us or taking away sorrow — that kind of mind control is unsettling for most of us. We are fiercely protective of the idea that our feelings originate inside of ourselves, that we are in charge here. So the idea that artificial happiness can be created by a computer that controls electrodes in our brain hooked to wires that snake down our neck? No thanks.
That sentiment is understandable, but it’s not what people with these implants experience. As I’ve talked with people who had lived first with devastating depression and then with these devices, I have come to think that these implants do not make a person feel artificial joy. “DBS is not going to give you happiness,” O’Neill says. Instead, “it just kind of clears the way.”
Overcoming misconceptions about what this technology can and can’t do is yet another burden for Jon and others. The patients I spoke with were incredibly candid about their depression and their treatment. They graciously tolerated my questions. But being open about their medical condition and treatment can exact a steep price.
If you or someone you know is facing a suicidal crisis or emotional distress, call or text the 988 Suicide & Crisis Lifeline at 988.
The next articles dives into the tough topic of stigma around mental disorders and their treatments.
This series was made possible with funding from the Alfred P. Sloan Foundation.







