Faulty Fountains of Youth
Adult stem cells may contribute to aging
Skin sags. Hair grays. Organs don’t work quite like they used to. A gradual wearing out and running down of the body’s tissues seems an inherent part of growing older. Rejuvenation of skin, muscles, and other body parts naturally declines with the passing years.

Scientifically speaking, however, this observation is much less self-evident. Some cells in a person’s body can resist the tide of aging. Consider the reproductive cells a person carries that will become the cells of newborn children who have 80-plus years of life to look forward to. Generation after generation, these reproductive cells form an unbroken line stretching for millennia.
The reason that an otherwise healthy person grows old and dies remains a mystery. Scientists have suggested several suspects for why people’s bodies wear out with age, including accumulated damage to DNA, free radicals, and the shortening of telomeres—the caps on the ends of chromosomes. While each of these factors may play a part, biologists acknowledge that their understanding of aging is incomplete.
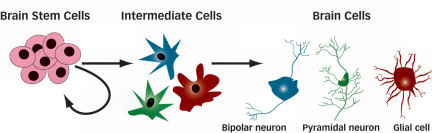
Enter stem cells. Scientists have long known that people have small reservoirs of stem cells in some of their tissues, such as bone marrow. These stem cells are distinct from those found in newly fertilized embryos—the more controversial embryonic stem cells. The embryonic type can become any type of cell in the body.
Adult stem cells, in contrast, can normally generate new cells only for the tissue in which they’re found: blood cells for blood, intestinal cells for the intestines. As old cells in these tissues are damaged or wear out, nearby stem cells can manufacture new ones to take their place. At the same time, the stem cells produce more copies of themselves, maintaining a seemingly indefinite pool of cells capable of churning out a stream of replacement cells.
Until recently, most scientists thought that adult stem cells existed only in tissues that need to constantly replace their cells, such as skin, blood, and the lining of the intestine. But over the past few years, researchers have found stem cells in many, perhaps most, of the body’s organs and tissues. Even the brain, which scientists once thought never replaced its nerve cells during adulthood, is now known to have stem cells that make new nerve cells throughout life (SN: 6/16/07, p. 376).
With the realization that so much of the body contains self-renewing stem cells, scientists began wondering whether changes in these stem cells over time might contribute to aging.
Imagine that, as a person ages, these fountains of cellular youth might start to run dry. As the supply of fresh cells dwindles, tissues would gradually decline and show signs of age. “That was the initial model” of how stem cells could be involved in aging, says Norman E. Sharpless, a stem cell expert at the University of North Carolina in Chapel Hill. And some data support this idea.
Graying of hair, for example, could be caused by a decline in melanocyte stem cells that accompanies aging, as observed by Emi K. Nishimura and her colleagues at Dana-Farber Cancer Institute in Boston. Melanocytes make the hair pigment melanin, so depleting these stem cells eventually causes loss of hair color, the team reported in Science in 2005.
Elderly people also have diminished resistance to disease because their immune systems make fewer of the disease-fighting white blood cells known as lymphocytes. In mice, bone marrow stem cells produce fewer lymphocytes as the mice get older, Derrick J. Rossi, now at Harvard Stem Cell Institute in Cambridge, reported in 2005 in the Proceedings of the National Academy of Sciences.
Yet evidence is mounting that the connection between adult stem cells and aging is more complex. Some kinds of stem cell actually grow more abundant with age. And just as stem cells affect aging, the aging body affects stem cells.
Tinkering with time
To untangle these effects, scientists led by Thomas A. Rando of Stanford University surgically joined pairs of mice like reconnected Siamese twins. The team linked the animals’ circulatory systems so that blood from each member of a pair flowed through both mice. One mouse in each pair was old; the other was young.
Scientists knew that the ability of muscle stem cells (also called satellite cells) to repair damaged muscles declines substantially with age. Rando’s team wanted to find out whether such declines should be attributed to changes in the satellite cells themselves or to changes in the cells’ environment as the animals aged.
“There clearly is an effect of aging on stem cells,” Rando says. “But I think the other question is … are those changes reversible or irreversible?”
Amazingly, the blood of the young mice completely restored the tissue-healing powers of the satellite cells in the older mice, Rando’s team reported in 2005 in Nature. Exposure to the young blood reactivated a system of proteins inside the cells called the Notch signaling pathway, which is crucial for triggering the cells’ muscle-repair functions. Notch signaling in satellite cells normally declines in old age, but Rando’s experiment showed that this decline is a response to changes in the blood, not the result of an inherent wearing out of the satellite cells themselves.
This influence of the cells’ environment is possible because all cells receive signals—including hormones and other messenger proteins—from their surroundings, and these signals allow the cells to behave appropriately for their context. So a change in these external messengers in aging mice could diminish the satellite cells’ muscle-repair activity.
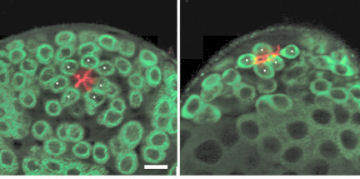
Stem cells’ surroundings also wield an influence in fruit fly testes. Changes in the stem cell–harboring niche inside the testes contribute to a decline in the number of sperm-making stem cells with age, according to research by D. Leanne Jones of the Salk Institute for Biological Studies in La Jolla, Calif., and her colleagues. As the flies grew old, the niche produced less of a protein that activates a gene in the stem cells called unpaired, which triggers self-renewal of the cells, the team reported in the Oct. 11, 2007 Cell Stem Cell.
“We definitely see changes in the environment long before we start to see” signs of intrinsic aging, Jones says. In mice testes as well, “there seems to be evidence for the environment aging instead of the stem cells themselves.”
In other cases, though, stem cell aging seems independent of context. Blood-forming stem cells from bone marrow age in an unusual way. When scientists transplant blood stem cells from an old mouse into a young mouse, allow the young mouse to grow old, and then repeat the process for several generations, the stem cells lose none of their ability to make copies of themselves. In fact, in some mouse strains, blood stem cells become even more numerous with age.
But that’s not necessarily a good thing. While old age doesn’t appear to affect blood stem cells’ power of self-renewal, it does gum up their ability to make specialized offspring cells. Ideally, each time a stem cell divides, one of the daughter cells would remain a stem cell, and the other would continue dividing to produce a fresh crop of specialized cells to replenish the tissue. That way, the stem cell’s lineage always contains only one stem cell at a time to replace the original, keeping the total number of stem cells constant.
For that number to increase, daughter cells must sometimes both become stem cells, decreasing production of tissue-replenishing cells.
Even when these elderly stem cells do spawn new lines of specialized cells, the process goes awry. Blood stem cells must give rise to a whole family of specialized cells: red blood cells, lymphocytes, monocytes, macrophages, and others. As the stem cells age, something goes wrong in this specialization process, skewing it away from making lymphocytes. So the old-age slump in germ-fighting lymphocytes happens not because the stem cells peter out but because they charge ahead with their specialization machinery slightly broken. In mice, this misbehaving of blood stem cells occurs even when scientists repeatedly transplant the cells into young animals, leading them to conclude that the stem cells themselves become damaged with time.
Fighting death with aging
In trying to understand how stem cells in various organs deteriorate with age, scientists have run up against the perennial nemesis of cell biology: cancer.
“Having all these cells around that can divide all the time is quite dangerous for an organism,” Sharpless says. Cells continually accumulate DNA damage, but copying and segregating the DNA during cell division is particularly hazardous. Every time a cell divides, there’s some error of replication.
Most of these mistakes get fixed by repair enzymes, but certain lingering errors in DNA can cause a cell to begin growing and dividing out of control, which is how cancer arises. Cells have elaborate tools for detecting DNA damage early and either fixing it or shutting down the affected cell. Recent data suggest that these mechanisms for thwarting cancer could cause the body to cull some of its own stem cell supplies.
For example, researchers led by Sean J. Morrison of the University of Michigan in Ann Arbor found a link between the decline in nerve stem cells in mouse brains and the potent anticancer gene p16. This gene causes cells to enter a dormant state called senescence. Mice bred without p16 retained significantly more of their nerve stem cells into old age than did mice that had the gene, Morrison’s team reported in Nature in 2006.
The famous tumor-fighting gene p53 also reins in damaged stem cells in old age. Blocking the activity of p53 in stem cells restored populations of intestinal stem cells in elderly mice, K. Lenhard Rudolph of Hannover Medical School in Germany and his colleagues reported in the January 2007 Nature Genetics.
Whether the bodily declines that come with aging are due to the depletion of stem cells depends on which organ is in question—and on which scientist you ask. Most scientists agree that adult stem cells play an important role in aging; the other thing that they seem to agree about is that this role is complicated. “There’s still a tremendous amount of debate about even the [blood stem cell] system, which is one of the best-studied systems,” Jones says.
In blood and other tissues with high cell turnover, decline of stem cells may make a greater contribution to the signs of aging than it does in tissues with slower cell turnover.
In skin, which constantly produces new cells, a decline in stem cell vigor is expected by some scientists to play a big part in the sagging and poor elasticity of skin that comes with old age. For organs such as the brain and heart, which retain most of their cells throughout adulthood, signs of old age more likely come from traditional mechanisms of aging acting on the organs’ mature, specialized cells.
But even this guideline may be too simple. Alzheimer’s disease, a form of dementia that commonly occurs in the elderly, is characterized by plaques accumulating in the brain. Young people’s brains make the plaque proteins as well, but some data suggest that immune cells called macrophages patrol the brain and clear out budding plaques. Macrophages are continuously being made by—you guessed it—blood stem cells. So even for organs in which cell renewal by stem cells proceeds very slowly, the declines of old age might be caused by the decline of adult stem cells elsewhere in the body.
Some aspects of aging will likely prove unrelated to stem cells, Sharpless says, but these cells now appear far more important for aging than scientists once thought. “I’ve stopped trying to predict which symptoms of aging are related to [stem cell] proliferation and which are not,” Sharpless says. Scientists “used to be so confident about this 10 years ago. Now I’m prepared to be wrong.”