At-home brain stimulation gaining followers
DIY head zappers hope to become better gamers and problem solvers, but the technology may not be ready for prime time

BRAIN HACK Brain stimulators have escaped the lab — ready or not — and people are juicing their brains from the comfort of home.
Eli Meir Kaplan
The first time Nathan Whitmore zapped his brain, he had a college friend standing by, ready to pull the cord in case he had a seizure. That didn’t happen. Instead, Whitmore started experimenting with the surges of electricity, and he liked the effects. Since that first cautious attempt, he’s become a frequent user of, and advocate for, homemade brain stimulators.
Depending on where he puts the electrodes, Whitmore says, he has expanded his memory, improved his math skills and solved previously intractable problems. The 22-year-old, a researcher in a National Institute on Aging neuroscience lab in Baltimore, writes computer programs in his spare time. When he attaches an electrode to a spot on his forehead, his brain goes into a “flow state,” he says, where tricky coding solutions appear effortlessly. “It’s like the computer is programming itself.”
Whitmore no longer asks a friend to keep him company while he plugs in, but he is far from alone. The movement to use electricity to change the brain, while still relatively fringe, appears to be growing, as evidenced by a steady increase in active participants in an online brain-hacking message board that Whitmore moderates. This do-it-yourself community, some of whom make their own devices, includes people who want to get better test scores or crush the competition in video games as well as people struggling with depression and chronic pain, Whitmore says.
As reckless as it sounds to juice a brain at home with a 9-volt battery and 40 dollars’ worth of spare parts, this technology’s buzz is based on legit science. Small laboratory studies suggest that carefully controlled brain stimulation can boost a person’s memory and math abilities, hone attention and fast-track learning. The U. S. military is interested and is funding studies to test brain stimulation as a way to boost soldiers’ alertness and vigilance. The technique may even be a viable treatment for pernicious mental disorders such as major depression, according to other laboratory-based studies.
Many of the scientists who are leading the charge, however, insist that this simple, relatively safe and cheap technology isn’t ready for home use. The research is too preliminary, and such stimulation may prove to be ineffective at best or, at worst, dangerous, some say. Certain kinds of stimulation may cause unintended harm; brain stimulation is not as foolproof as many people would like to believe.
Still, “humans have a long history of playing with their brains,” says neuroscientist Vincent Clark of the University of New Mexico and the Mind Research Network, a nonprofit neuroscience research institute in Albuquerque. And it’s unlikely that scientists’ protests will change that. Right now, scientists, policy makers and DIYers are all wrestling with whether — and how — the technology should be regulated.
Ethical quandaries as well as questions about efficacy and safety call for restraint. But demand, fueled by tantalizing news of promising studies, has largely drowned out those cautionary calls. “We are in such a fog of ignorance,” says neuroethicist Hank Greely of Stanford Law School, who studies how brain research intersects with society. “We really need to know more about how this works.”
The promise
The brain traffics in electricity. Minuscule electrical bursts create the signals that allow people to think, remember and feel, so it makes perfect sense that external electricity might influence how the brain operates.
That insight isn’t new. A physician to the Roman emperor Claudius eased headaches by placing a live, electric torpedo ray (similar to a stingray) onto the heads of long-suffering patients. In the 11th century, electric catfish were proposed as treatment for epilepsy. In the 1800s, the nephew of Italian bioelectrical pioneer Luigi Galvani, who harnessed lightning to make dead frogs’ legs jump, used electrical stimulation to treat people’s melancholia.
Today’s burgeoning field of “electroceuticals ” takes advantage of the same principle. Clinicians use various delivery methods — both external and implanted — to transform the brain’s electrical activity. For some people, electroconvulsive therapy can ease severe depression or mania that drugs don’t touch. This wallop of electricity sparks a short seizure that’s thought to reset the brain and lessen symptoms. Some people with Parkinson’s disease have also found relief in electricity: Rhythmic zaps from electrodes implanted deep into their brains can reduce tremors and rigidity.
Those methods are different from the one that has captured the attention of the DIY crowd. Transcranial direct current stimulation, known as tDCS, sends small amounts of stable electric current into the scalp. Although the details are still hazy, tDCS is thought to work by coaxing nerve cells to become either more or less active, depending on whether the anode or the cathode of the device is placed over the neurons. The electricity doesn’t compel neurons to fire off messages or stay silent; instead, it gently tips the scales toward action or inaction, studies have found.
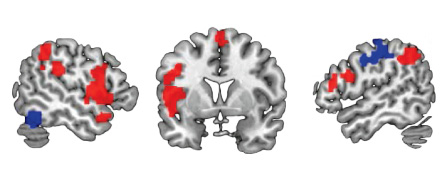
Depending on which part of the brain gets nudged, tDCS can influence things like attention, working memory, visual abilities and mathematical skills. For instance, stimulation to the top of the brain caused 15 healthy people to learn a made-up number system better than healthy people who received no stimulation, and the benefit lasted months after the stimulation stopped, neuroscientist Roi Cohen Kadosh of the University of Oxford and colleagues reported in Current Biology in 2010.
tDCS may also alleviate symptoms of depression, other small studies suggest. In a randomized trial of 120 people with moderate to severe depression, tDCS, with positive stimulation (anode) over the left side of the brain and negative (cathode) over the right, boosted the effects of the drug sertraline, or Zoloft, scientists reported in 2013 in JAMA Psychiatry. Over a six-week period, people who received both tDCS and sertraline scored on average 11.5 points better on a depression rating scale than people who received placebos. (A drop of three points was considered clinically relevant.) tDCS alone caused a smaller drop — 5.6 points — versus sham, and sertraline alone caused an even smaller drop: 2.9 points less than placebo.
Other more wide-ranging effects of electricity may be involved. tDCS appears to influence the behavior of large cohorts of neurons. Even more generally, electricity can influence blood flow in the brain, inflammation and probably a whole range of other processes.
Despite an incomplete understanding of the technology, clinicians have already taken note of the findings, particularly the antidepressant effects of tDCS. Several clinics offer tDCS therapy to patients, often outside of research studies.
Some people, however, don’t want to go to the trouble of visiting a doctor or enrolling in a lab study to experience tDCS. Prefab tDCS machines can be purchased online for a few hundred dollars or less. DIY plans for building a tDCS system are available to anyone with an Internet connection. So people are making their own.
“I have a graduate student whose background is in philosophy, and he was able to build one in an afternoon for less than $50,” says neuroscientist and ethicist Peter Reiner of the University of British Columbia in Vancouver. “The device is shockingly simple, and a little scary because of that.”
Enter the DIYers
No one really knows how many people use this technology at home, Greely says. His Stanford colleague Anita Jwa sent a questionnaire to participants in online tDCS chat groups, and heard back from about 120 respondents. The survey is anything but comprehensive, but it attempts for the first time to study the DIY community, which Jwa found is overwhelmingly male, and not necessarily young. About 23 percent of respondents were 40 or older, the survey revealed. “It’s not just the pimply kid in the basement playing a massive online role-playing game,” Greely says.
In fact, many of the people who use tDCS have an illness that hasn’t been treated successfully and are trying it out of desperation, says Brent Williams, who maintains a tDCS website. With a background in engineering, Williams had no trouble building a unit for himself and his wife. They use it to boost their creativity and memory, among other things.
Williams, who directs an educational outreach program at Kennesaw State University in Georgia, became convinced that the technology can change lives. He began to proselytize about it on his website. “I get e-mails every day from people who are doing tDCS stuff,” he says. “A lot of those e-mails come from, frankly, pretty desperate people who live in countries or regions where they don’t have access to the doctors that we have access to. They are desperate to do tDCS for depression or chronic pain or whatever the case may be,” he says.
That idea — people turning to tDCS instead of working with a doctor or using tDCS regularly to improve performance — worries some scientists and physicians. Notably, most of the scientists who regularly zap subjects’ brains in their labs aren’t likely to use the technology on their own brains, according to a study published in the July-August Brain Stimulation. Of 287 researchers who study noninvasive brain stimulation (including but not limited to tDCS), only 8 percent said they juice themselves. Common reasons for abstaining included believing the benefit was too small and concern about safety.
The perils
And those 8 percent of researchers probably used adequately tested machines to deliver an appropriate dose of electricity. Home use is only as good as the person who builds and operates the system. Just ask the people who have posted online images of scalp burns from improper current.
Burns and even more severe reactions, such as reports of manic episodes and even temporary paralysis caused by brain stimulation, seem to be rare. “It’s not like people are dropping dead or having their teeth fall out,” Greely says.
In a 2013 paper in the Journal of Neuroscience, Cohen Kadosh and a colleague reported that the math gains people experienced from experimental stimulation weakened a different math skill. “We can improve one function but it comes at the cost of another function,” he says. It’s entirely possible that other deficits brought about by tDCS have remained hidden because not many people have looked for them.
Assuming safety wasn’t an issue, there are plenty of reasons a person at home wouldn’t achieve the same results as participants in a carefully done lab study, says Cohen Kadosh. The best brain locale to stimulate is probably different in every person. Depending on culture, expertise and age, people rely on different parts of their brains to do math, for instance. Plus, brain regions can be found at slightly different physical coordinates from person to person.
The question of dose isn’t settled, either. Many studies use about 20 minutes of 1 to 2 milliamps of current at a time. But the effect of that dose may vary widely from person to person. Antidepressants can change the brain’s baseline excitability, as can other drugs, both legal and illicit. Age, sex and smoking status have all been linked to differences in brain behavior. And the movement of electrical current can be influenced by wrinkles in the brain, the thickness of the skull and the shape of the head. These individual quirks shift the goal line, making it nearly impossible for someone at home to know exactly where and how long stimulation should be applied.
For years, Cohen Kadosh has meticulously researched how best to safely and effectively transmit electricity to the brain. But even he has qualms about using tDCS. “People are adults. They’re free to do whatever they want,” he says. “But I would not do this myself.”
To regulate or not?
The fact that the desire for this technology is running ahead of adequate safety and efficacy studies is something that Cohen Kadosh has become acutely aware of during his research with tDCS. “I’ve been contacted in the past by parents who want to improve their children’s performance in order to get into an excellent university or be better in school,” he says.
Philosophically, external brain stimulation is no different than making a child take piano lessons, Greely says, so long as the technique is proven safe and effective. And that’s a big caveat. “I know enough about brains to know that they’re really complicated,” he says. Without a firm understanding of how the brain works, Greely is loath to start meddling with his. “At this point, I wouldn’t encourage my kids to do it,” he says.
Right now, it’s perfectly legal to build or buy a tDCS system. The $249 tDCS headset called “foc.us” is advertised as a tool to “excite your prefrontal cortex and get the edge in online gaming.” And Thync, a company that’s developing a headset to “shift your state of mind,” claims it will allow users to tailor their moods, creating energized, relaxed or focused experiences.
The independent, nonprofit Institute of Medicine in Washington, D.C., will hold a workshop early next year to explore the role of external brain stimulation in society. Discussions, sponsored by a collection of federal agencies, patient groups, industry and nonprofits, will include potential benefits and risks of the technology, regulatory quandaries and ethical dilemmas such as whether it’s acceptable to use the technology for cognitive enhancement in healthy people and the implications of involuntary or coercive use.
For his part, Williams, the Georgia DIYer, has written about how to safely and ethically use tDCS and has even suggested a code of safety standards for fellow DIY users. His rules include seeking out a medical professional for advice, treatment and follow-up, never using tDCS alone and never using the technology on children or animals.
It’s not clear whether tDCS will really take off and become the next killer app, Greely says. But as the science hums along, people will probably keep pushing the technology’s boundaries. That means scientists’ cautious “Don’t try this at home” may continue to fall on deaf ears and tingling scalps.
This story appears in the Nov. 15, 2014 issue with the headline, “Brain Hack: Consumers take their neurons into their own hands.”

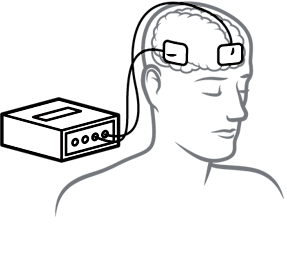 Electrodes are placed on the scalp sending weak electrical current (usually between 1 and 2 milliamps) into the brain. Depending on the placement and type of stimulation, users may alter working memory, attention or math skills. Depression and chronic pain may also be reduced, some studies suggest.
Electrodes are placed on the scalp sending weak electrical current (usually between 1 and 2 milliamps) into the brain. Depending on the placement and type of stimulation, users may alter working memory, attention or math skills. Depression and chronic pain may also be reduced, some studies suggest.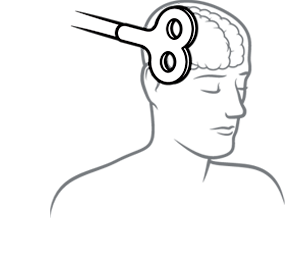 A coil of wire held next to the head generates a magnetic field, triggering electric currents in the brain. TMS has shown promise as a way to treat psychiatric disorders and provide cognitive boosts. The Food and Drug Administration has OK’d versions of TMS for depression and migraines.
A coil of wire held next to the head generates a magnetic field, triggering electric currents in the brain. TMS has shown promise as a way to treat psychiatric disorders and provide cognitive boosts. The Food and Drug Administration has OK’d versions of TMS for depression and migraines.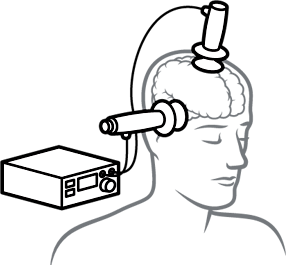 Once a patient is under anesthesia and given a muscle relaxant to prevent movement, electrodes are placed on the head to send about a 500 to 900 milliamp current through the brain, sparking a brief seizure. ECT is used to treat severe depression, bipolar disorder and schizophrenia.
Once a patient is under anesthesia and given a muscle relaxant to prevent movement, electrodes are placed on the head to send about a 500 to 900 milliamp current through the brain, sparking a brief seizure. ECT is used to treat severe depression, bipolar disorder and schizophrenia.