A malaria vaccine with live parasites shows promise in a small trial
Next steps include figuring out whether the results hold up in larger trials
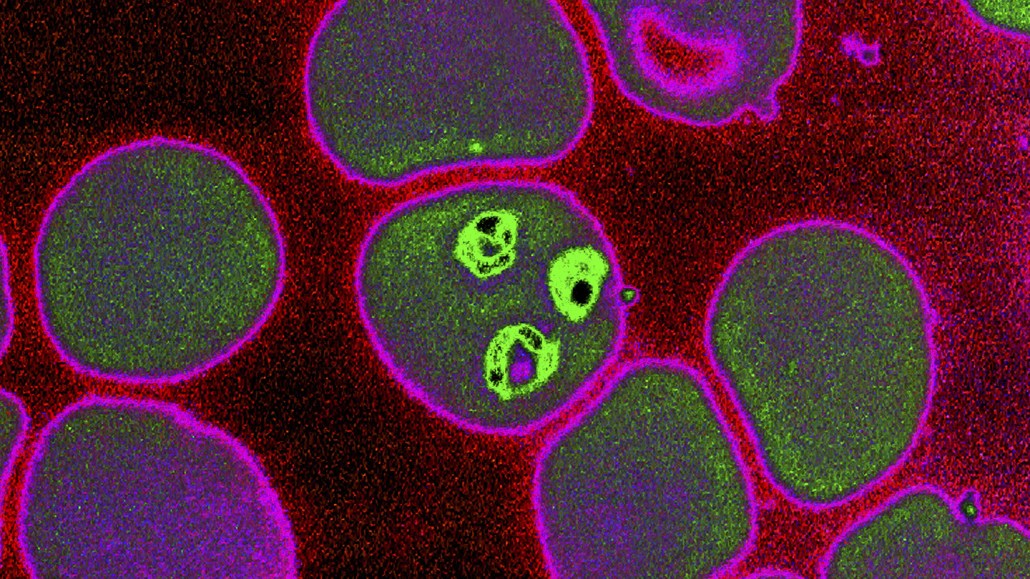
A malaria vaccine that combines a shot of live Plasmodium falciparum parasites that cause the disease with a dose of drugs to curb the infection has shown promise in a small trial. The parasite (shown in bright green) gets its start in the liver and then spreads to the blood.
James Cavallini/ BSIP SA / Alamy Stock Photo
In a one-two punch, a malaria vaccine in development pairs a shot of the live parasite that causes the disease with a whammy of infection-fighting drugs to immediately quell it.
The candidate is the latest vaccine to show promise against a formidable foe, bolstering hopes that an effective shot might be on the horizon. Malaria, a disease caused by the parasite Plasmodium falciparum, affects more than 200 million people around the world every year. In 2019, an estimated 409,000 people died from the mosquito-borne disease, 67 percent of whom were children younger than 5.
The live parasite vaccine and drug combo showed 87.5 percent efficacy in a small group of healthy adult participants, researchers reported June 30 in Nature. The live parasite shot — which is followed by a dose of one of two anti-malarial drugs to eliminate the infection — not only protected people from the same strain included in the vaccine, but most people could also fend off a different parasite strain that circulates in Brazil.
If the results hold up in a larger study, “it would be fantastic,” says Wilfred Ndifon, a mathematical biologist at the African Institute for Mathematical Sciences in Kigali, Rwanda, who was not involved in the study. Even as newly emerging diseases like COVID-19 have killed millions and martialed global attention and resources, “we are still falling short of controlling the ones that already exist,” Ndifon says.
Currently there is only one malaria vaccine, called RTS,S, in use in Africa that provides partial protection in young children. Rather than live parasites, the shot uses a key malaria protein that helps the parasite infect liver cells to train the body to recognize the pathogen. In a late-stage clinical trial, it prevented 39 percent of malaria cases among children 5 to 17 years old. Now, it’s given to children in Ghana, Malawi and Kenya as part of a pilot program through the World Health Organization.
Another malaria vaccine candidate called R21 was designed to improve protection by helping the body better home in on attacking that same malaria protein. That jab recently showed 77 percent efficacy among 450 children in Burkina Faso, researchers reported May 15 in the Lancet.

Still, the world is in desperate need of good malaria vaccines. And using live organisms to protect people is “the oldest way of making a vaccine,” says Patrick Duffy, a malaria vaccine researcher at the National Institute of Allergy and Infectious Diseases in Bethesda, Md. Shots for diseases like measles and chickenpox also rely on using live, albeit weakened, viruses to teach the immune system what to attack.
In the new study, Duffy and his colleagues gave 44 healthy people in the United States three intravenous doses of the vaccine spaced about a month apart. Another 12 people were included as controls. Two or three days after the shot, vaccinated participants took one of two anti-malaria drugs — pyrimethamine and chloroquine — to weaken and eliminate the parasite.
Taking anti-malaria drugs is a crucial part of the vaccination process. That’s because “these malaria parasites in the vaccine are fully infectious,” says David Cook, an infectious diseases physician also at NIAID. “If we weren’t to give [participants] any medication at all, people would develop a malaria infection.”
When P. falciparum infects a new host, sporozoites — the life stage of the parasite that is transmitted from mosquitoes — first attack the liver. Then the parasite bursts into the bloodstream, infecting red blood cells and causing symptoms like fever, headache or chills. Pyrimethamine curbs the infection in the liver; chloroquine tackles parasites in the blood. So while participants who got chloroquine might develop malaria symptoms, those who get pyrimethamine wouldn’t, Cook says.
A low-dose vaccine with around 51,200 sporozoites followed up with chloroquine protected four out of five participants when they were exposed to the parasite three months after the last dose. A dose of pyrimethamine protected only two out of nine people.
Increasing the amount of parasite in each dose to 200,000 sporozoites, however, bolstered immune defenses. Seven out of eight people, or 87.5 percent, who got a high-dose shot and then took pyrimethamine were protected when exposed to the same parasite strain three months later.
The higher dose shot also worked against another malaria parasite strain from Brazil, protecting six out of six people who took chloroquine and seven out of nine people given pyrimethamine. That type of cross protection is important because malaria is a diverse parasite, says Kirsten Lyke, a vaccinologist at the University of Maryland School of Medicine in Baltimore. So people need to mount an immune response that can recognize multiple strains, not just the one included in a vaccine.
Still, because the trial was so small, there’s “some degree of uncertainty about whether this approach to vaccinating is highly effective,” Ndifon says. What’s more, getting people to come back to the clinic for three doses plus drug treatments will be a challenge, both Ndifon and Lyke say.
Some experts “see this as a traveler’s vaccine,” more accessible to those who have the time and resources to follow up with the treatment, says Adrian Hill, a vaccinologist at the University of Oxford and director of the Jenner Institute who is involved with the R21 malaria vaccine. “If you give people [in Africa] a whopping dose of malaria and then for any reason that drug is expired or it isn’t the right drug or they took it too late — who’s going to take responsibility for that?” What’s more, the shot must be stored in liquid nitrogen and is “impossible to [manufacture] at the scale you need to make an impact on malaria” in areas where it naturally circulates, Hill says.
Ideally anti-malarial drugs like chloroquine and pyrimethamine would be given at the same time as the shot to minimize the chances people will miss treatments, Duffy says. The team has plans to test that regimen in upcoming trials, as well as figure out how long protection might last.







