A mutation that helped make a laboratory version of the H5N1 bird flu transmissible through the air nearly obliterates the ability of the virus to latch onto avian cells. At the same time, the mutation slightly boosts the virus’s ability to infect human cells, an international team of researchers reports April 24 in Nature.
The finding follows up on controversial research published last year that transformed the H5N1 virus, a microbe usually restricted to birds, into one that could spread between ferrets through the air (SN: 6/2/12; p. 20; SN: 7/14/12, p. 8). Some scientists and policymakers questioned whether such research should be done at all. Others argued that the work could help spot viruses poised to become pandemic strains and might point to vaccine targets.
The new study shows that a mutation can have different effects in different flu strains, something that might not have been discovered without the earlier research.
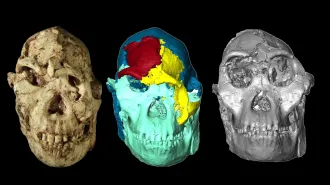
In the course of transitioning from a bird flu to a human disease, influenza viruses generally develop a preference for grasping sugar molecules called receptors on the surface of human cells. One common mutation that helps viruses do that, called Q226L, changes an amino acid in the hemagglutinin protein — the molecule that gives the virus the H in its name. Hemagglutinin acts as a grappling hook to snag cells, making easier for the virus to infect them. The Q226L mutation, which occurs in the experimental H5N1 work and in natural influenza strains that caused pandemics in 1957 and 1968, twists the hemagglutinin protein to better hang onto human cells.
Usually virus strains with the mutation retain some power to hold onto bird cells, but not in the case of H5N1, says structural biologist and study coauthor Steven Gamblin of the MRC National Institute for Medical Research in London. The single amino acid alteration flips the H5 hemagglutinin from a protein with a high affinity for avian cells and almost none for human cells to one that clings weakly to human receptors but cannot get any handle on bird receptors. The mutant H5 binds human sugars 200 times more strongly than it does bird receptors, Gamblin and his colleagues found.
The mutant H5 gets only the weakest of holds on human sugars, says Ram Sasisekharan, an MIT biochemist who has conducted similar studies on other influenza viruses. Its grip does not rise above a threshold typically needed for other flu viruses to infect human cells, making the role of the mutation in transmissibility a mystery. “It’s very confounding,” he says.
But Gamblin speculates that the virus’s abandonment of its avian past may allow it to evade components of human mucus called mucins, which are structurally similar to avian receptors. Normally, mucins glom onto flu viruses and tie up the grappling hooks, preventing hemagglutinin proteins from latching on to cells. Because the Q226L mutation destroys hemagglutinin’s ability to recognize bird receptors, it may allow the virus to slip past the mucins and get right to cells, aiding in transmission, Gamblin says.
This mutation also carries a potential upside for people: Because the mutant H5 can no longer bind to avian cells, viruses carrying the mutation probably would not be able to replicate in birds, Gamblin says. That could mean that the mutant virus may not be able to jump directly from birds into people. Instead, to pick up the mutation and become transmissible by air, H5N1 would first have to infect — and reproduce in — people or another animal. So far, only the laboratory created strains of H5N1 can spread through the air, and they contain other mutations that adapt the virus to live in mammals.