Normal 0 false false false MicrosoftInternetExplorer4 Get rid of DNA-altering viruses — check.
In a crucial step toward realizing medical treatments based on embryonic-like stem cells, researchers have found a safer way to revert adult mouse cells to an embryonic state. The new technique, reported online September 25 in Science, avoids using viruses that alter the cells’ DNA, a major goal among stem-cell researchers since these DNA mutations can lead to cancer.
Such reprogrammed cells could sidestep the controversy surrounding therapies based on embryonic stem cells, many scientists believe, because the embryonic-like cells can be made from a person’s skin or blood cells without creating or destroying an embryo. Coaxing these reprogrammed cells into becoming, say, fresh heart or pancreas cells for transplantation back into the patient could offer new, personalized ways to treat ailments such as heart disease and diabetes.
Until now, reprogramming adult cells in lab dishes required infecting the cells with viruses that carry the four reprogramming genes. Although the scientists cripple the viruses so that they can’t replicate, the viruses can still insert these four genes directly into the cells’ DNA at random locations. These willy-nilly changes to the cells’ DNA could disrupt the cells’ own genes, occasionally in ways that cause the cells to grow out of control and form a tumor. In addition to this risk, any process that alters a cell’s DNA complicates government approval for medical use.
The new technique overcomes these problems by using a different kind of virus that does not alter the cells’ genetic code, researchers report.
“None of the cells that we produced had any evidence of any virus left” after reprogramming, says Matthias Stadtfeld, coauthor of the study and a molecular biologist at Massachusetts GeneralHospital in Boston.
The safer virus carries the same four genes into adult cells — Oct4, Sox2, Klf4 and c-Myc — but instead of inserting those genes into the cells’ genetic code, the virus lets the genes free-float within the cells. Proteins encoded by these genes do the actual reprogramming, and the cells’ protein-making machinery can read the four genes even if they’re adrift in the cells. Eventually, the cells degrade the genes, and the viruses get lost as the cells repeatedly divide.
“It’s very exciting because it’s the first demonstration of [reprogrammed] cells without viral integration,” comments Robb MacLellan, a stem cell expert at the David Geffen School of Medicine at the University of California, Los Angeles. “It’s a proof of concept.”
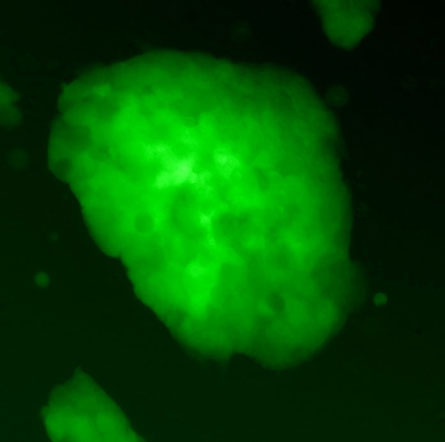
More research is needed before the technique could be used for medical therapies. Stadtfeld and his colleagues reprogrammed skin and liver cells from adult mice. Because they used mouse cells, the scientists could perform the ultimate test for whether the resulting reprogrammed cells possessed the quintessential trait of embryonic stem cells, the ability to become any type of cell in the body. That test is to insert the reprogrammed cells into mouse embryos and allow those embryos to grow into adult mice. Just as true embryonic stem cells would, these reprogrammed cells gave rise to all types of cells in every organ of the adult mice’s bodies.
The question remains whether the reprogramming feat will work for human cells, but many scientists expect that it will. “It’s likely that it will be able to be shown in human cells,” MacLellan says.
Reprogramming worked for only one of every 100,000 to 1 million cells, a conversion rate about 10 to 100 times worse than that for DNA-altering viruses. Conversion worked for the liver cells, but skin cells (which would be much easier for doctors to obtain from patients) needed a small cheat for the reprogramming to work: The researchers inserted one of the four genes into the cells’ DNA.
Stadtfeld says the team doesn’t know yet why the skin cells needed extra help, or why the conversion rates were so low. These two problems must be solved before reprogrammed cells could be used for medical treatments.
Even then, scientists will still need to improve other techniques for coaxing these cells into heart, pancreas or other cell types needed for therapies. These lab techniques are still under development and will probably take longer to perfect than the reprogramming methods will, Stadtfeld says. “I think it will take at least five or 10 years, because you have to be really careful before you transplant anything.”
Normal 0 false false false MicrosoftInternetExplorer4 Normal 0 false false false MicrosoftInternetExplorer4






