Tiny blood vessels expel clots by force
Mouse study uncovers new way capillaries keep flow going
Tiny blood vessels in the brains of mice have a novel way of dealing with clots — they pack them up and shove them out, right through the vessel wall. This never-before-seen clearance maneuver, reported May 27 in Nature, gets blood flowing again and prevents cell death in nearby brain tissue.
The new study also found that as mice age, their ability to evict clots deteriorates. Unchecked blockages in small vessels can cause tiny areas of damage to the brain, a process that may be related to the onset of age-related dementia.
Researchers suspect the same kind of clot clearance might happen in humans. “Our vessels are being cleared up on a minute-by-minute basis, which is a great new finding and very exciting,” comments neurologist Costantino Iadecola of the Weill Cornell Medical College in New York City, who was not involved in the study.
Until now, researchers knew of only two ways for blood vessels to dispel clots: Pulsing blood could simply wash the clot away or clot-busting enzymes could dissolve it. These tactics usually work well in large vessels, but small vessels have a harder time pushing clots along. Microvessels, which include capillaries, have diameters of about 20 micrometers or less, leaving them vulnerable to blockages by just a few dead blood cells, a little chunk of cholesterol or a calcium plaque.
“These are tiny vessels — anything can block them,” says study coauthor Jaime Grutzendler of Northwestern University’s Feinberg School of Medicine in Chicago. When tiny clumps get lodged in a microvessel, blood flow stops, which can lead to tissue damage and cell death — a dangerous thing in the brain.
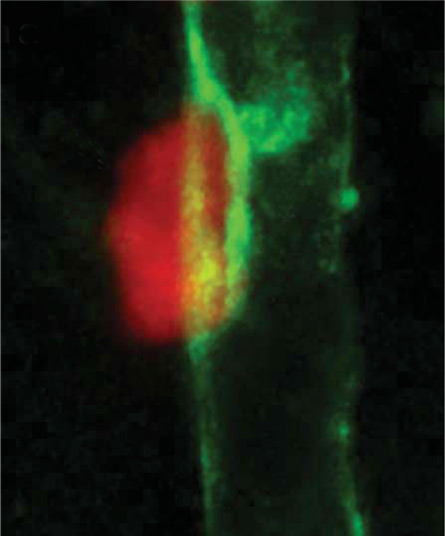
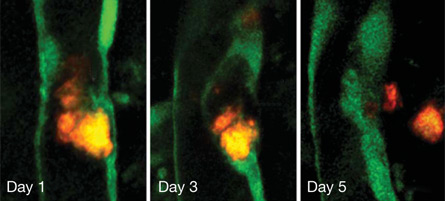
To see how microvessels handle clots, Grutzendler and colleagues injected small, fluorescently labeled clots made of plastic, globs of cholesterol or a sticky protein called fibrin into mice’s carotid arteries. Then the researchers watched as the clots traveled into microvessels in the brain. After two hours, about half of the clots had cleared, the team found. But the remaining clots seemed stuck.
Over the next two to seven days, the researchers saw something completely unexpected. New tissue began to grow and envelop the clot, then a hole opened up in the vessel wall and the membrane-packaged clot was shoved out of the vessel and into the brain. The innermost clot-surrounding membrane patched up the vessel wall, and blood flow started up again. Microvessels were able to expel all three kinds of injected clots, although the expulsion of plastic clots took longer.
In further experiments, the team found that old mice aren’t able to expel clots as well as young mice. More clots clogging microvessels means more brain damage. Such damaged spots are so small that they may not be noticed, but they could add up, Grutzendler says. “Small inefficiencies in this system could have damaging effects over decades,” he says. “We’re hypothesizing that this could be a very underestimated cause of dementia.”
Whether the same clot-expelling process happens in human brains is still an open question. Researchers don’t know how many microclots occur in the human brain, nor do they know how harmful those clots are. Neurologist Patrick Pullicino of the University of Kent in England says that conceivably, such clots could cause cognitive impairment if the brain is bombarded with them. In fact, doctors know that the risk of dementia rises after a person has undergone open heart surgery, which often produces a “shower” of small clots, but the link between microclots and cognitive decline is not clear.
The hope is that once researchers understand the clot-expelling process better, they might be able to enhance the process with drugs. But Iadecola cautions that researchers are a long way from knowing how to do that. “Vascular diseases of the brain are very complex. All kinds of things are imposing on each other. At the end, you don’t know who’s doing what.”







