Ultrasound attacks Alzheimer’s plaques
With aid from microglia, treatment in mice helps improve memory
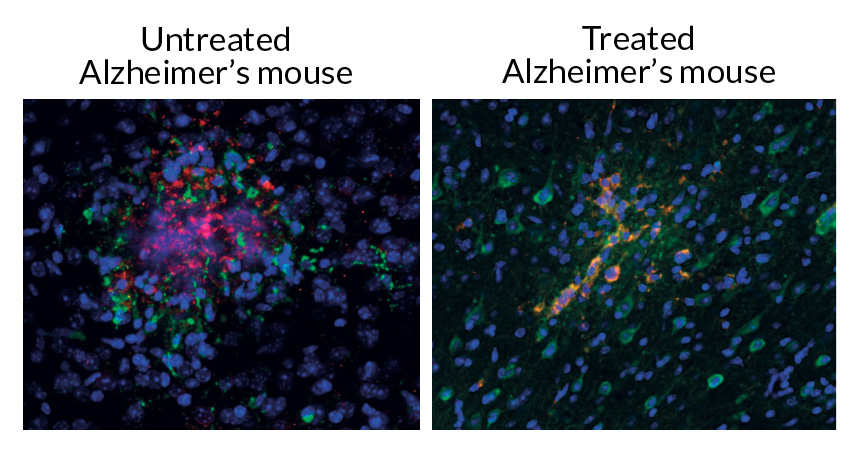
SWALLOWED WHOLE In the brains of mice treated with ultrasound (right), the nervous system’s immune cells (green and blue), take in more bits of plaque (red) related to Alzheimer’s disease than they do in the brains of untreated mice (left).
Leinenga and Götz/STM 2015
Using high-frequency sound waves to rev up tiny air bubbles in the brain appears to treat symptoms of Alzheimer’s disease in mice. The findings suggest that a similar technique could one day be used to treat the disease in humans.
Scientists in Australia injected microscopic bubbles into the blood vessels of the mice and then moved an ultrasound beam over the animals’ foreheads. The treatment reduced brain deposits of a plaque linked with Alzheimer’s disease. That change in the brain may have helped the diseased mice perform better on a series of memory tests, the researchers report March 11 in Science Translational Medicine.
“This is a great paper building up on our story that ultrasound can reduce plaques associated with Alzheimer’s,” says neuroscientist Isabelle Aubert of the Sunnybrook Research Institute in Toronto. The results, she says, validate work she and colleagues published in 2013 showing that the blood contains natural molecules, such as antibodies and antioxidants, that may help clear Alzheimer’s-related plaques from the brain, if those molecules can cross the blood-brain barrier.
“The blood-brain barrier is a major impediment to treating any diseases of the brain because it restricts almost all molecules from passing from the blood into the brain,” says neuroscientist Gerhard Leinenga of the University of Queensland in Brisbane, Australia.
In the new study, Leinenga and Jürgen Götz, also at Queensland, looked at how the ultrasound treatment affected a strain of mice that were genetically engineered to make dangerous levels of amyloid-beta, bits of a plaque implicated in Alzheimer’s that can damage and kill nerve cells. Diseased mice that got the treatment over their entire forehead five times over six weeks had roughly 50 percent less plaque in the cortex, the outer layer of the brain, than diseased mice of similar ages that did not receive treatment.
Leinenga and Götz suggest that the treatment allows molecules found in the blood, but normally absent from the brain, to cross the blood-brain barrier. The molecules then appear to turn on microglia — white blood cells in the brain and spine that engulf and digest toxins. The experiments show that the treated mice’s microglia had consumed twice as much amyloid-beta plaque as untreated mice. Cultured microglia cells also swallowed more amyloid-beta when given albumin, an antioxidant in the blood.
That finding about albumin may help scientists understand how the body and brain can work together to clear plaques related to Alzheimer’s disease, Aubert says.
In the new study, mice treated with ultrasound also performed better than untreated mice in a series of tasks, including remembering how to avoid shock zones on a rotating floor, spontaneously exploring a Y-shaped maze and investigating a new object in a set they had seen before.
“We were somewhat surprised that the ultrasound treatment improved the memory of the mice,” Leinenga says, explaining that memory may improve when amyloid-beta is removed from the brain.
Aubert, however, argues that the improvement in memory may not be solely from the clearance of the Alzheimer’s-related plaques in the cortex. Instead, she says, the ultrasound treatment could actually spur the development of new nerve cells the hippocampus, a brain region responsible for learning and memory. Last year, she and colleagues showed the treatment had this effect in healthy mice.
Leinenga says there are a number of caveats to address before this treatment is ready to try in humans. The human brain and human learning and memory are much more complex than in mice. The human brain is much larger than a mouse brain, and the skull is also much thicker, so the treatment will need to be adapted for these differences. Leinenga and Götz are working to scale up the treatment to test in sheep first.







