Why people with celiac disease suffer so soon after eating gluten
T cells in those with the autoimmune disorder rapidly dump immune chemicals into the blood

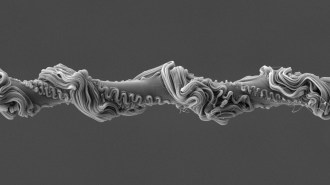
TUMMY TROUBLER People with the autoimmune disorder celiac disease sustain damage to their small intestine when they eat gluten. The only remedy is a gluten-free diet, but new research pinpointing the source of the problem may lead to future therapies.
Stephen Barnes/iStock/Getty Images Plus