Some koalas in Australia have rebounded their numbers from a small pool of individuals. Their genes are now catching up, restoring the genetic variation that was lost.
mscaus/iNaturalist Australia
A rapid koala rebound in southeastern Australia is also boosting their genetic variation, showing one way out of an extinction death spiral.
After nearly disappearing from the region over a century ago, the marsupials’ recovery has come with increased reshuffling of genes, enhancing their long-term chances of adaptation and survival. The findings, published March 5 in Science, provides hope for species starting over.
By the early 1900s in the Australian state of Victoria, the number of koalas (Phascolarctos cinereus) had fallen to as few as 500 individuals due to pressure from the fur trade. To protect the larger Victorian population, people moved handfuls of them to nearby islands. The small island populations grew throughout the 20th century and so scientists moved some koalas back to the mainland to help bolster that much reduced population. Victoria’s koala population swelled to nearly half a million by 2020, but they were the descendants of small groups of forebears that lacked genetic diversity.
These kinds of genetic bottlenecks in a species’ history may increase the risk of inbreeding and its negative effects. “That’s where you get deformities, poor health, things of that nature,” says Collin Ahrens, an evolutionary biologist at Cesar Australia, an independent environmental research company in Brunswick.
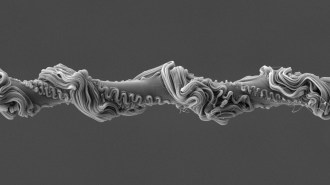
Ahrens and his colleagues wanted to know how genomes had changed in koalas during this type of whiplash recovery. The team analyzed a database containing the genetic instruction books of 418 koalas from 27 populations across eastern Australia. It estimated the timing and degree of each population’s fall and rise in numbers, and how different measures of genetic variation had changed in response.
Populations in Victoria showed the echo of their brush with extinction: Their genetic diversity was low. But that was just part of the story.
As the population quickly grew and more mating occurred, it led to newer and varied genetic combinations along with new mutations, some of which can be beneficial. There still wasn’t much underlying variety in the genes compared with other populations. But the mixing and matching increased the changes that offspring could inherit beneficial genes without harmful ones. Already, tooth and testicle malformations have been reduced in the Victoria koalas, possibly from a change in the population’s genetic makeup.
“All that genetic information is being mixed up in a lot of different new combinations,” says Ahrens. “In the north, we have a completely different picture.” There, koalas have higher genetic diversity, but they’re now entering a genetic bottleneck as their populations dwindle.
In a way, the Victoria koalas’ genetic resurgence is like what’s sometimes found in invasive species. Such species rapidly balloon in numbers from a handful of individuals, similarly accumulating new mutations and variation as they interbreed. An example is the Roesel’s bush cricket (Metrioptera roeselii): A small number of individuals in Sweden regained a larger population’s genetic diversity in just 15 generations.
Cock van Oosterhout, an evolutionary geneticist at the University of East Anglia in England, says the findings match what evolutionary theory has predicted for recovering populations. “However, empirical data is still rare, and it is encouraging to observe this directly in a wild species,” he says.
The findings show that at least under some circumstances, species larger than just crickets can emerge out of seemingly catastrophic genetic bottlenecks and start regaining the same degree of variation that was lost. Starting with low diversity doesn’t mean that the species will be limited by its genetic toolkit. Ahrens thinks this realization may change how conservation genetics is performed by researchers in the future.
“I think this [research] has a message of hope,” says Ahrens.
Ensuring rapid, sustained population growth can reduce inbreeding risk fast, van Oosterhout agrees. But he and his colleagues have also seen dogged genetic issues in recovered bird species like whooping cranes and Seychelles paradise flycatchers. Rapid population growth may be like first aid for a species’ recovery, but other more targeted approaches like intentionally modifying genes may help get species fully out of the woods, he says.