Boosting estrogen, only in the brain
Selective transformation of protein into sex hormone could limit side effects
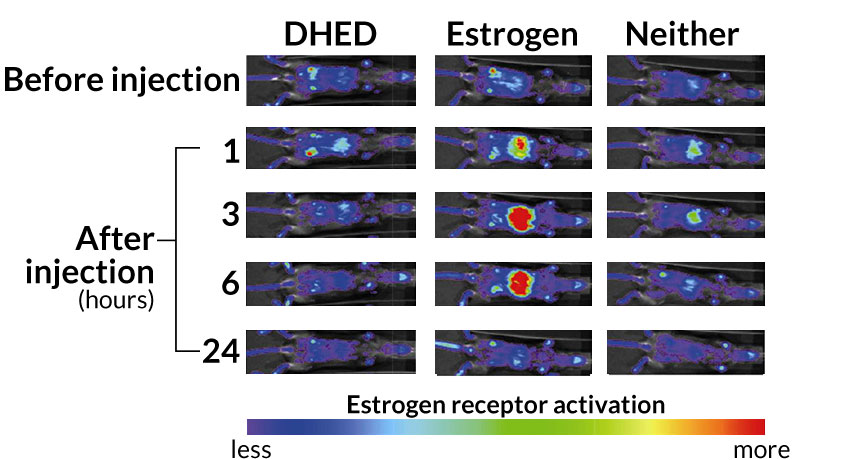
TARGETED EFFECT The chemical DHED produces the hormone estrogen in the brain, but not the body. In mice with tissues genetically modified to light up when exposed to estrogen, pure estrogen produces a bright glowing around the internal organs (center). But mice given DHED (left) do not light up more than untreated mice (right), indicating that DHED does not become estrogen in their bodies.
L. Prokai et al/Science Translational Medicine 2015
- More than 2 years ago
Researchers have developed a chemical that transforms into a powerful hormone once inside a rat — but only in the brain, not the body.
A protein in rats’ brains turns a chemical nicknamed DHED into the hormone estrogen, scientists report July 22 in Science Translational Medicine. This targeted treatment could provide estrogen to the brain and avoid potentially dangerous side effects in the body, the researchers say.
“This is an interesting breakthrough,” says neuroendocrinologist Bruce McEwen of the Rockefeller University in New York City. The idea of treatments that affect the brain but not the body, or the body but not the brain, could be useful in treating a number of conditions, including cancer, he says. But the implications of this study for hormone replacement therapy in women is up for debate, a number of researchers say.
In menopausal women or those who have had their ovaries surgically removed, lack of estrogen in the brain can cause symptoms such as hot flashes and sleep disturbances. Taking estrogen can relieve those symptoms but can cause side effects in the rest of the body, including an increased risk of certain cancers.
The chemical DHED is nearly identical to natural human estrogen, but it has an extra oxygen atom. A specialized protein found in rodents’ brains recognizes the chemical and chops off the oxygen, turning DHED into estrogen. The body’s other organs lack this protein, so they can’t turn DHED into estrogen, says study author Laszlo Prokai, a chemical biologist at the University of North Texas Health Science Center in Fort Worth.
In female rats that had their ovaries removed, DHED led to a measurable increase of estrogen in the brain, but not in the uterus or bloodstream, Prokai and colleagues report. In mice genetically modified so their tissues light up when exposed to estrogen, DHED lit up only the animals’ brains; estrogen, but not DHED, caused the mice’s internal organs to light up. And unlike estrogen, DHED did not appear to stimulate the growth of human breast cancer cells in culture.
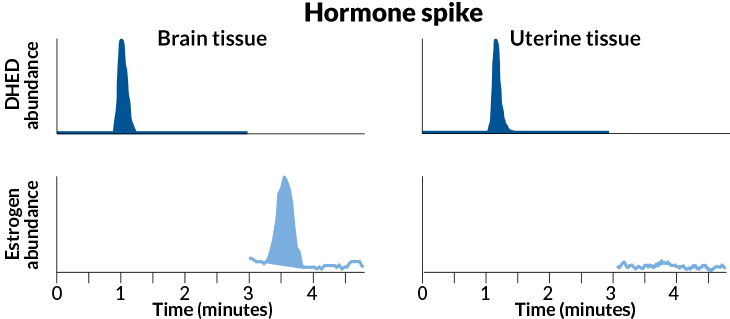
Story continues below infographic
Identity change
In a rat’s brain (left), the chemical DHED (dark blue) is rapidly converted into the hormone estrogen (pale blue). But in the uterus (right), this transformation doesn’t happen.
Credit: L. Prokai et al/Science Translational Medicine 2015
In a simulation of hot flashes, rats undergoing morphine withdrawal experienced temporary increases in skin temperature on their tails. DHED-turned-estrogen decreased this temperature increase in rats just like doses of actual estrogen did, says study coauthor Istvan Merchenthaler, a neuroendocrinologist at the University of Maryland School of Medicine in Baltimore.
Prokai and Merchenthaler believe that the chemical could someday be used to treat humans for neurological symptoms associated with estrogen deficiencies — not only hot flashes, but also depression and anxiety.
Other scientists say the mechanism for turning the chemical into the hormone is intriguing, but question the advantages of a brain-only treatment when it comes to estrogen.
“This is an interesting area of research, and I think it does warrant further study,” says endocrinologist JoAnn Manson of Harvard Medical School and Brigham and Women’s Hospital in Boston. But, she says, it remains unclear if estrogen can help treat mood disorders like depression.
“The jury is still out on the effects of estrogen on cognition,” she says. “The trial results have been mixed.” Manson also notes that in the human body, estrogen protects bone and heart health — benefits that would be lost if estrogen was produced only in the brain. It may be more important to understand ways to maximize the health benefits and minimize the risks of full-body estrogen treatment, she says.
Estrogen itself often behaves differently in animals and humans, says neuroscientist and psychiatrist Natalie Rasgon of the Stanford School of Medicine. “We have tens of thousands of papers on very positive effects of estrogen in animals and in the dish. We do not see similar results in humans,” she says. “It’s a very complex biology.”
Longer-term studies of DHED’s effect on the body would also be required, says Lila Nachtigall, a reproductive endocrinologist at New York University Langone Medical Center. “It might have some potential down the line, but it needs an awful lot of work,” she says.
Still, if DHED is in fact proven to affect only the brain, it could have huge implications in treating a variety of brain disorders, Rasgon says. “This sounds very promising.”