A brain at rest offers clues to Parkinson’s, Alzheimer’s
PET scans pick up clear signs of breakdown in neurological networks
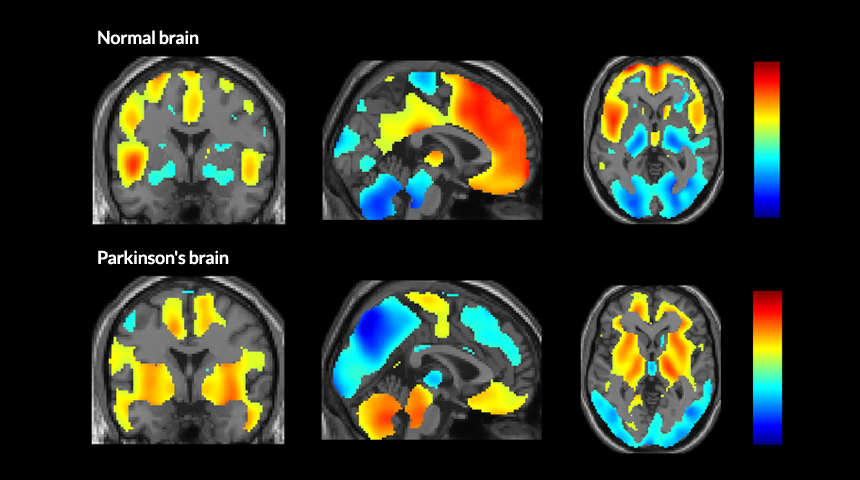
NETWORKING Brain scans reveal the part of the brain that’s active (red shows most activity; blue shows least) when people are not thinking about anything in particular. In healthy people (top row), these coordinated areas of the brain are called the default mode network. But in people with mild to moderate Parkinson’s disease (bottom row), a new, abnormal network takes over.
P. Spetsieris et al/ PNAS 2015, adapted by S. Egts







