Five big questions about when and how to open schools amid COVID-19
It’s time to layer up defenses to keep kids as safe as possible when they head back to class

Teacher Chablis Torres reads to children wearing masks and sitting at desks spaced far apart in a summer pre-school class in Monterey Park, Calif.
FREDERIC J. BROWN/AFP/Getty Images
It’s back-to-school time in the United States, but for the world’s leader in coronavirus infections and deaths, what “back to school” means is anything but clear.
Many countries have gotten ahead of the pandemic with extensive testing, tracing and quarantining. That tight control means that children in Denmark, Singapore and China have returned to school, with extra safety measures.
The situation is fundamentally different in the United States. No other country has attempted to send children to school with coronavirus infection levels as high as they are in some parts of the country. Many large school districts, including those in Los Angeles, Atlanta and Houston, will begin the school year with all kids learning from home. Other districts have yet to announce their plans, which may include models that mix in-person learning with remote classwork.
School districts have been struggling to make the call, given a lack of data on how to reduce risk. Two major scientific societies have provided some guidance. On June 25, the American Academy of Pediatrics strongly recommended that policy decisions be made with the goal of having children in school, in person. The National Academies of Science, Engineering and Medicine agreed, urging in a July 15 report that to the extent possible, in-person education should be prioritized, particularly for young children and those with special needs.
Doing so in a way that minimizes risk will come at a hefty price. The National Academies’ report estimated a price tag of $1.8 million for an average U.S. school district with around 3,300 students. That would pay for personal protective gear such as masks, hand-washing stations, cleaning supplies and extra staff so that students could be spread out. Of course, even if a district spends the funds, there are no guarantees that students, teachers and staff won’t get sick.
The price of keeping students home is harder to quantify, and could be even greater. In addition to missing out on academic and social growth, some kids in lockdown face greater risks of abuse, neglect and hunger. And to go smoothly, remote learning requires reliable internet service, a safe place to work and adults standing by to help. That kind of support is impossible for many families, particularly those with parents or caregivers who can’t work from home.
Here, experts weigh in on five of the biggest questions on when and how to reopen schools, if not safely, then as safely as possible.
Is there a “safe” level of COVID-19 for reopening schools?
Unfortunately, there is no threshold level of COVID-19 spread in a community that guarantees the safety of sending kids back to school. But if SARS-CoV-2 is under control, that reduces the risk that there will be outbreaks when schools reopen.
Schools “are a microcosm of the community,” says Wendy Armstrong, an infectious disease physician at Emory University School of Medicine in Atlanta. “What happens in there reflects what’s going on elsewhere.”
Communities can use three basic metrics for assessing the virus’s spread: COVID-19 cases, hospitalizations and how many tests for SARS-CoV-2 are coming back positive. There are no magic numbers for these metrics, Armstrong says; instead of looking at one day or one value, it’s important to look at trends over the course of two weeks. “If your trends are not coming down, then there’s a problem,” she says.
The World Health Organization has an extensive list of public health criteria to consider before reopening a community at large. Among them is a rate of positive SARS-CoV-2 test results of less than 5 percent in the previous two weeks.
This number, called the positivity rate, is one way to tell whether a state or county is doing enough testing. On August 4, only 16 states plus the District of Columbia were equal to or below 5 percent positivity on average over the previous week, according to the Johns Hopkins Coronavirus Resource Center.
Some states, including Delaware and Oregon, have announced conditions they expect to see before schools can reopen. Oregon Governor Kate Brown said on July 28 that among other requirements, counties must meet two criteria three weeks in a row: a positivity rate of 5 percent or less and 10 or fewer cases per 100,000 residents in the preceding seven days.
But even if SARS-CoV-2 is well under wraps in a community, that doesn’t mean the work is done. Infection control measures are still necessary. Denmark and Norway, where community spread was low, avoided outbreaks by limiting class size and student interactions, among other steps. But in Israel, where curbs on class size were brief, a high school with crowded classes that let students remove face masks during a heat wave suffered a large outbreak, researchers report online July 23 in Eurosurveillance.
What is known about kids transmitting the virus at school?
Children can certainly transmit the coronavirus, says Aubree Gordon, an epidemiologist at the University of Michigan in Ann Arbor. “But it seems fairly clear that, at least for young children, they probably transmit less” than other age groups. The details of how or why, however, are a moving target.
Some of the latest studies emerging from other countries tell conflicting stories. A study tracing nearly 60,000 contacts of 5,706 COVID-19 patients in South Korea, for instance, revealed that 10- to 19-year-olds may transmit the virus more like adults, researchers from the Korea Centers for Disease Control and Prevention reported online July 16 in Emerging Infectious Diseases. But kids younger than 10 appeared less likely to pass the virus on to others — infecting only 5.3 percent of contacts living in the same home. But kids are more likely to have mild disease or be asymptomatic, so they can easily be overlooked as transmitters, Gordon says. A preliminary study from Italy, posted online July 29 at medRxiv.org found that children younger than 15 were more likely to transmit the virus than older age groups.
When children do get sick, they appear to carry plenty of virus. A preliminary study of symptomatic people, posted July 19 at medRxiv.org, found that children have the same amount of virus in their bodies as adults do during an infection. Another small study found that children younger than 5 have even higher amounts of the coronavirus’ genetic material in their upper respiratory tract than older kids or adults do, researchers report July 30 in JAMA Pediatrics.
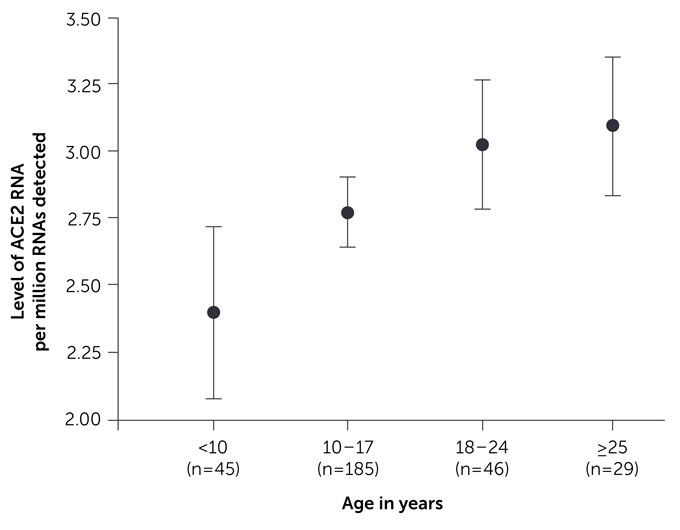
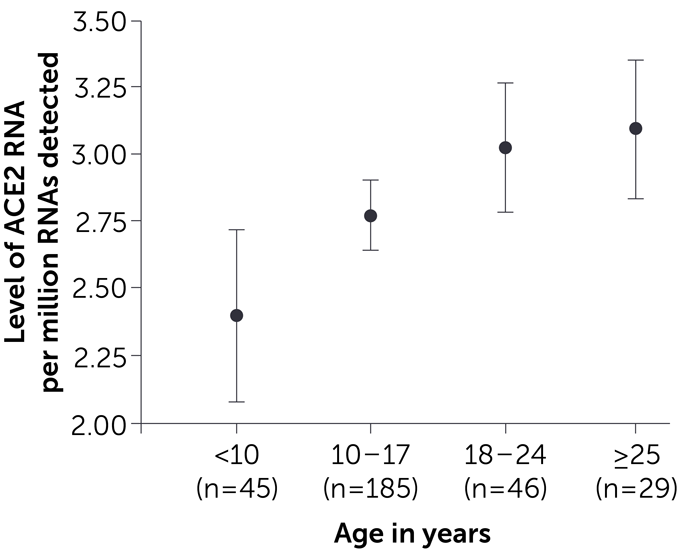
But because kids most often have mild COVID-19 symptoms or are asymptomatic, perhaps they don’t cough as much and therefore release less virus into the air around them. The reason kids don’t often get sick is also still unclear, although younger children may have lower amounts of the protein that the viruses hijacks to break into cells, called ACE2, in their upper respiratory tracts than older kids or adults, researchers report May 20 in JAMA. That could mean children younger than 10 might have fewer susceptible cells for the coronavirus to infect.
Despite all this, the number of COVID-19 cases in children is going up across the United States. As of July 23, state-level data compiled by the American Academy of Pediatrics and Children’s Hospital Association showed that children represented 8.4 percent of all U.S. COVID-19 cases — up from 3.7 percent in mid-May. That increase could be because more kids are now getting exposed (SN: 6/3/20), or because they are only now being widely tested.
Any school that opens will want to know when the virus is spreading within the student body. One solution is to test all kids at regular intervals, with those testing positive quickly notified and kept home. But schools largely lack the infrastructure for that much testing, and in many places, getting results back can take over a week.
“It’s just not going to be feasible in most areas of the country,” says Tina Tan, a pediatric infectious disease specialist at Northwestern University in Chicago. The U.S. Centers for Disease Control and Prevention does not recommend universal testing of all students in its latest guidelines for schools. Instead, the agency suggeststesting only students with COVID-19 symptoms and those who have been in contact with a confirmed case.
“The onus is going to be on families to keep kids at home if they have symptoms of any kind,” says Sandra Albrecht, a social epidemiologist at Columbia University. Schools must also keep an eye on the community, says Jennifer Nuzzo, an epidemiologist at the Johns Hopkins Center for Health Security in Baltimore. If cases spike, schools may have to close again.
Should schools open all at once?
Some countries have adopted a staged, gradual approach, allowing elementary schools to reopen for in-person education sooner than middle or high schools, for instance.
Denmark allowed children up to age 12 to go back to school first. Similarly, Norway began with day cares and preschools, and then progressed to first through fourth grades before allowing older kids to return to school. Those strategies make sense, some researchers say, since young children seem to be less likely to get sick or to spread COVID-19. Also tipping the scales in favor of school for the elementary school set: Young children aren’t able to participate in remote learning as well as older children.
Communities can also link their reopening stages to infection rates and kids’ needs. For instance, Uruguay allowed children in less-populated areas to return to school first, before adding in disadvantaged kids and then high-school seniors.
Then there’s the hybrid model — some days in school, some learning from home. “On its face, it seems like maybe that’s a good idea,” says exposure and risk scientist Joseph Allen at Harvard T.H. Chan School of Public Health, because it could help space out kids and reduce their time with others. “But when you start to dig down into it, you realize that it’s a flawed strategy that’s not based on any empirical evidence or data.”

Many children would be mingling with other people on their off-school days, then bringing those exposures back into classrooms. In some cases, younger kids would have relatively fewer contacts if they were in school five days a week in stable groups, Linda Darling-Hammond, an education researcher and president of the Learning Policy Institute in Palo Alto, Calif. From a virus-spreading standpoint, she says, various mixtures of settings “would be much more dangerous, frankly.”
Would it help to group kids in bubbles or pods?
In March, people were asked to stay home to flatten the upward curve of coronavirus infections. By shrinking our social spheres, we could block the virus’ spread. That led some people to form small groups with little outside interaction. The same strategy can be used in schools.
“If you have kids in one classroom or one pod that do get sick, it doesn’t spread like wildfire through the school,” Allen says. A bubble or pod also makes it easier for contact tracers to track exposure. If a child or teacher tests positive, the bubble can be quarantined instead of the whole school.
Bubbles are easiest to form in elementary schools, where classes usually include a stable group of kids and a teacher, Darling-Hammond says. Large high schools pose more challenges, but “the same principle would hold even in a high school of 2,000,” she says, with 100 students sharing four teachers and a counselor, for instance.
Denmark and Norway have adopted the pod strategy for elementary school students, in addition to reopening schools in stages. And in Canada’s hard-hit Quebec province, some students will return to school bubbled into groups of six.
“The smaller the bubble, the better,” says computational epidemiologist Daniel Klein of the Institute for Disease Modeling in Seattle. An unpublished simulation of school children in Washington State, created by Klein and colleagues, found that bubble sizes of about 20 students and one teacher created a “significant benefit,” he says. The researchers haven’t yet been able to model the effects of other bubble sizes.
But to be effective, kids have to stay in their bubbles. Situations like after-school care and bus rides could foil the bubble benefits. “The bubble bursts very quickly, as soon as you start bumping into other people,” Darling-Hammond says.

What physical changes can schools make to reduce risk?
Schools can reduce risk that infections will spread by focusing on three major categories: airflow, reconfiguring the building interior to enable social distancing and hygiene.
Encourage airflow. There’s mounting evidence that coronavirus can linger in the air in aerosols — small respiratory droplets people generate when they talk or breathe (SN: 7/7/20). Students and teachers in schools will be doing plenty of talking and breathing (SN: 4/2/2020), so dilution of classroom air with fresh air from outside is critical, explains L. James Lo, who studies building ventilation at Drexel University in Philadelphia.
Unfortunately, many school ventilation systems aren’t up to the task of bringing in enough fresh air, Lo says. Most systems already operate near capacity, and would be expensive to upgrade. So one option might just be to purchase smaller air cleaning units with good filtration and a high air flow rate. “For a very large room … it’s not feasible … but if you have a small office you could purchase a portable air cleaner that has good filtration and flow rate,” Lo says.
Another place with a lot of fresh air? Outside. Outdoor classes “could be ideal; there’s precious little evidence of transmission outside,” says Ed Nardell, a pulmonologist at Harvard Medical School.
Keep the distance. Public health experts recommend that people stay at least six feet apart, which can be hard to do in schools. Some schools are trying to spread people out, by limiting class sizes and setting up one-way hallways so that people walk “next to each other, not facing each other,” Lo says. The less people can breathe in each other’s faces, the better.
Some experts suggest keeping high schoolers working remotely at home and using the high school buildings to spread out the elementary students.
Then there’s the bus, another social distancing challenge. More than half of schoolchildren take the bus to school. And many parents don’t have the means to chauffeur kids to and fro. So bus riders need to wear masks and socially distance, which calls for a drastic increase in the number of buses and routes.
When it comes to physical barriers, masking is a must, but also a challenge for children. “Because [masks are] so uncomfortable, there has to be consideration of length of day,” says Rainu Kaushal, a health services researcher at Weill Cornell Medicine in New York City. “If you can get four hours every day with a mask on but can’t get six hours, schools need to think about that.” That might mean young children would go to school only for half a day, if that’s how long they can tolerate a mask. Kaushal also advised building in mask breaks, times when kids could run around outside — where transmission is less likely — with their masks off.
The CDC also recommends partitions and sneeze guards. “You definitely impede the transmission between people” with partitions, Lo says, “but you need to devise a very strong … cleaning strategy” because particles will deposit on those surfaces.

Clean everything. Hand hygiene is very important, and soap, sinks and alcohol-based sanitizers need to be in good supply. The entire classroom should be cleaned daily — desks, chairs, everything. “I would err on the side of multiple cleanings a day,” Kaushal says. Every effort will help. “It’s a layering of our defenses.”
One last layer: Children should be up to date on their vaccines — all vaccines. “You don’t want to have an influenza outbreak on top of a COVID outbreak,” Tan says.
All of this is daunting, but Americans can take some lessons from other nations. “Something like 20 countries have successfully reopened,” Kaushal says. In a June 30 JAMA Health Forum article, she and her colleagues drew lessons from those successful school opening. “I think it can be done,” she says.
There is no federal plan to track the spread of the virus in U.S. schools. Reopening schools during a pandemic will be a massive collection of experiments, carried out by thousands of school districts making decisions independently. Only time will tell whether some of these efforts will work.