CRISPR gene editor could spark immune reaction in people
Having antibodies against Cas9 ‘molecular scissors’ is common, study suggests
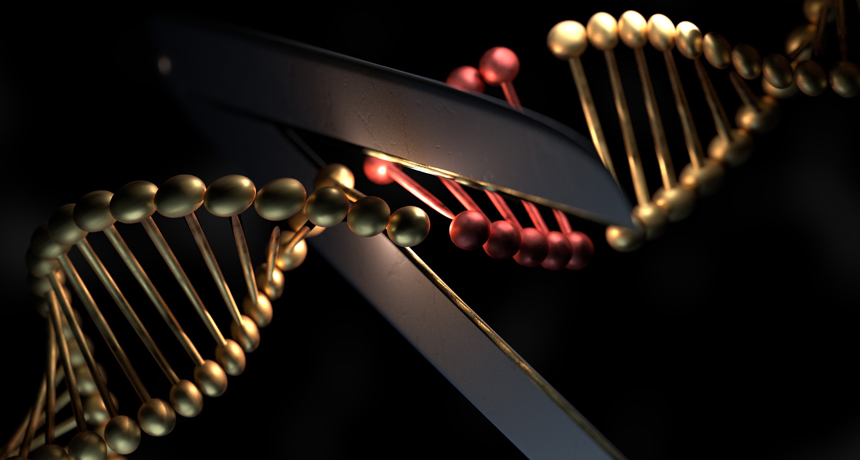
TECHNICAL DIFFICULTIES Scientists doing gene editing need to be aware of potential immune system attacks against a DNA-cutting protein.
tdhster/shutterstock