Like many women with parents of the Mad Men generation, Susan Murphy grew up in a household full of cigarette smoke. Both dad and mom smoked heavily, even while Murphy was still in her mother’s womb.
“That explains a lot,” Murphy quips, poking fun at herself.
But Murphy isn’t worried about her own health. She’s fine. Her children aren’t, though. One boy died of cancer as a toddler. Another has autism. And her daughter has attention deficit disorder. Murphy knows the scientific evidence isn’t in yet, but she still can’t help wondering whether their fates might have been affected by her exposure to tobacco smoke before she was born.
Murphy, a researcher at Duke University, studies links between a mother’s diet and chemical exposures during pregnancy with the child’s later health. She and others have established that the womb is the antithesis of Las Vegas; what happens there not only doesn’t stay there, it can influence a child’s health for life.
Now, animal studies and a smattering of human data suggest such prenatal effects could reach farther down the family tree: The vices, virtues, inadvertent actions and accidental exposures of a pregnant mother may pose health consequences for her grandchildren and great-grandchildren, and perhaps even their offspring.
Scientists have long known that radiation or certain chemicals can cause typos in a developing fetus’s genome — his or her genetic instruction book. Such mutations can get passed along to future generations in the DNA of sperm or egg cells. While exposure to sex hormones or a high-fat diet in the womb doesn’t directly change or damage DNA, those sorts of exposures can induce scribblings in the genome’s margins that can also be passed down.

The resulting health effects are not produced by altering DNA itself. Rather they stem from changes in chemical tags on DNA or its associated proteins, or to actions by RNA, another type of genetic molecule. All of these are exactly the types of changes that scientists have always assumed cannot be inherited. Their very name, epigenetic, literally means “over and above” or “beyond” genetics.
When these changes are inherited, scientists have found, the implications can be staggering. Part of your risk of disease may be determined by what your great-grandparents ate, not just the genes they passed on. Some researchers even believe that the long-lasting effects of these chemical marks helped shape human evolution.
Stuck for generations
Investigating how those marks travel to future generations is a new twist in the field of epigenetics. Originally, epigenetics researchers focused on the developmental processes that allow individual cells to specialize despite the fact that all the cells have the same DNA. It turned out that chemical tags that get stuck to DNA or to the proteins around which DNA is wound can influence gene activity without altering the genes themselves.
Some of those chemical tags highlight passages in the genome, typically so that particular genes will be turned on. Other tags work more like a censor’s black marker, redacting some genes so that they will be shut off. Chemically underscoring or crossing out different combinations of genes creates the various types of cells that populate the body.
Until fairly recently, scientists have thought that every new generation starts with its own freshly printed genome, devoid of epigenetic embellishments. That’s because shortly after fertilization, vestiges of epigenetic tags hanging from the DNA of eggs and sperm are wiped away, leaving a clean slate. New marks are made as the embryo develops, and over the course of a lifetime some can change. But then scientists began to document cases in which inheritance of a particular trait did not follow the usual rules of genetics, hinting that at least some epigenetic marks may be carried on to new generations.
Michael Skinner was among the first to document that certain chemicals could produce health effects across multiple generations without altering DNA. Exposing a pregnant rat to chemicals that disrupt the action of sex hormones could produce fertility problems that lasted at least to her great-great-grandchildren’s generation, his group reported in Science in 2005. Those problems were transmitted through the male line, apparently by way of chemical tags called methyl groups on DNA. (Many researchers study DNA methylation because it is more easily examined than other epigenetic tags, of which there are many.)
“At first everybody thought this was the greatest thing since sliced bread,” recalls Skinner, of Washington State University in Pullman. “But then the implications started to sink in.”
One implication is that epigenetic programming becomes permanent and gets passed along to future generations. Partly because it raises the specter of Lamarckian inheritance of acquired characteristics (think of the giraffe straining to reach high leaves and thus passing on longer necks to its offspring), the idea was not popular with many classical geneticists. To establish the idea that epigenetic marks can last generations, it was necessary to show that various chemicals and experiences could induce specific changes that had heritable health consequences.
Clues emerge
Evidence supporting that idea appeared in Nature in 2010. Rat fathers that ate a high-fat diet and became obese before mating passed along a propensity to become diabetic to their daughters (but not their sons), researchers in Australia reported.
Something in the dads’ high-fat diet apparently caused a change in methyl tags on DNA in the fathers’ sperm that was then passed on to the daughters. It was direct evidence that diet or other environmental factors could influence epigenetic marks in sperm, escape the epigenetic reset at fertilization and affect the health of offspring.
In people, babies born to obese fathers had an altered epigenetic legacy, Murphy and her colleagues reported February 6 in BMC Medicine. The children of 16 obese men had lower levels of methylation of the gene IGF2 compared with the kids of normal-weight dads.
Murphy and others have shown that smoking and other prenatal encounters can coincide with changes in epigenetic tags. But she remains cautious about saying that epigenetic marks can really be inherited. Instead, the changes may result from an exposure that directly affects multiple generations. After all, a developing fetus experiences nearly the same things as its mother does. Female fetuses already have their lifetime supply of eggs, so those eggs — the pregnant mother’s future grandchildren — are also directly affected by whatever mom encounters. Males don’t start making sperm until puberty, but the germ cells that will give rise to sperm are present in male fetuses and may also be affected by the womb’s environment.
So epigenetic changes observed in grandchildren might stem from conditions encountered by fetal germ cells. It’s not until the great-grandchild generation that researchers can determine whether an epigenetic mark is truly inherited, because that is the first generation that had no contact with what the original pregnant mom encountered.
Few studies, even in animals, have followed epigenetic marks for that many generations, says Leena Hilakivi-Clarke, a breast cancer researcher at Georgetown University in Washington, D.C.
Hilakivi-Clarke’s lab has studied the effects that hormones in the womb, such as estrogen and its chemical mimics, may have on breast cancer risk after menopause. Now her team is investigating breast cancer risks over multiple generations.
A legacy of cancer
Only about 10 percent of breast cancers that run in families can be linked to genetic mutations. While she was on maternity leave, Sonia de Assis, a researcher in Hilakivi-Clarke’s lab, began to wonder if the other 90 percent of cases might be explained by epigenetic inheritance. She got the idea after reading one of Skinner’s studies. It had shown that exposure to a fungicide could cause at least four generations of health problems in rodents.
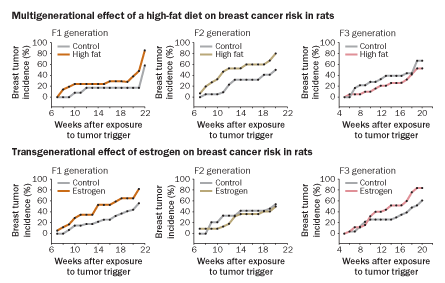
Back in the lab, de Assis convinced Hilakivi-Clarke that they should study multiple generations of rats to see if DNA methylation patterns that had been linked to breast cancer risk could be passed to future generations. The team exposed pregnant mother rats to things that influence breast cancer risk in humans: high-fat diets or ethinyl estradiol, a synthetic estrogen used in some birth control pills.
Pregnant rats on a high-fat diet had daughters and granddaughters that were more susceptible to developing mammary tumors when encountering a cancer-causing chemical later in life, the researchers reported last September in Nature Communications. But great-granddaughters were not at increased risk, indicating that when high-fat diets alter breast cancer susceptibility it is not a permanent, inherited change, says Hilakivi-Clarke.
Ethinyl estradiol, on the other hand, raised breast cancer susceptibility in the daughters, granddaughters and great-granddaughters of pregnant rats given the hormone in the last week of pregnancy (roughly equivalent to the last trimester in humans). In breast tissue, daughter rats exposed to the synthetic estrogen while in the womb had 214 genes with more methyl tags and 161 genes with fewer methyl tags than normal. That pattern persisted through the granddaughter on to the great-granddaughter generation, indicating that not only the risk of breast cancer but also the associated epigenetic marks could be inherited.
Estrogen isn’t the only chemical that can pass its health effects down through generations. Researchers in Skinner’s lab tested the effects of a variety of chemicals on ovarian health in rats. The team exposed pregnant rats to doses of chemicals people might encounter in everyday life. One was vinclozolin, the fungicide that gave de Assis the idea for her experiments. Among the others were various components of plastics, including bisphenol A; pesticides such as permethrin and the mosquito repellent DEET; dioxin; and jet fuel.
All of the chemicals studied led to an increase in ovary problems, including fewer eggs and more cysts, that lasted at least until the great-granddaughter generation, Skinner’s team reported in May 2012 in PLOS ONE. The increase in ovarian disease was accompanied by persistent changes in DNA methylation patterns in ovarian tissue.
Some of the treatments led to 100 percent of the great-granddaughters developing ovarian cysts. “There is no genetic mechanism that will give you that level of disease. None,” says Skinner. “Some of our phenomena are so robust we couldn’t explain it with genetics even if we wanted to.”
Skinner thinks that epigenetics offers an organism a way to adjust the activity of genes rapidly in response to environmental cues. Epigenetic marks prepare future generations for the environment that they are likely to encounter, he contends. He even thinks that epigenetic changes may eventually become permanently inscribed in DNA, thus influencing the evolution of species. “I don’t want to suggest that genetics and DNA is not important — it’s just not the whole story,” he says.
Flagged by RNA
Neither Skinner nor anyone else can yet explain exactly how epigenetic information gets passed to the next generation. But new clues are emerging from studies of worms and flies, and they point to a role for DNA’s chemical cousin, RNA.
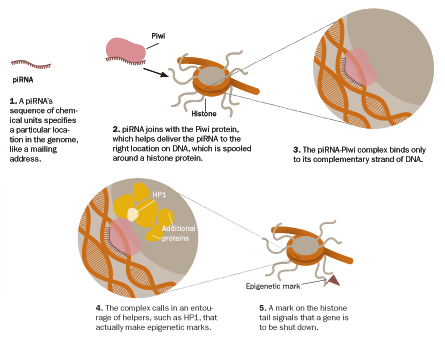
One of RNA’s jobs may be to establish where and how densely epigenetic tags are placed. Geneticist Erik Miska and colleagues stumbled onto RNA’s secret occupation while investigating an antiviral defense system in tiny, transparent worms called C. elegans. When viral genetic material infects a worm cell, an army of small bits of RNA attacks and neutralizes the threat. About 60 to 80 percent of offspring in each subsequent worm generation “remember” to shut off the viral genes or retain immunity to viruses. Miska’s team traced this memory to small RNAs called piRNAs (pronounced “pie RNAs”) found in germ cells.
When piRNAs trigger the shutdown of a gene, it’s permanent, the researchers reported last July in Cell. “It is 100 percent efficient in all the offspring and it continues to act forever, which is very weird,” says Miska, of the University of Cambridge in England. Forever, in this case, is at least 30 generations, as far out as his team looked.
Perhaps it should not be surprising that RNA can institute an everlasting change in gene activity. Plant geneticists have known for years that similar RNAs can permanently shut down genes, a process known as paramutation. Paramutation is the process that produces multicolored corn kernels, for instance. But it wasn’t thought to take place in animals. Miska’s data, and a 2012 Nature study showing that piRNAs can shut down genes in fruit flies, suggest that the little RNA snippets may be agents of enduring gene control in animals.
Miska’s team discovered that piRNAs’ takedown of certain genes is accompanied by another type of epigenetic mark, a methyl group stuck to a histone protein. Histones spool DNA so that it will fit inside cells, and also help control how active genes are. The histone mark linked to the piRNA-inactivated genes is known to dial back gene activity. In worms, that may be enough for permanent change.
Scientists are uncovering molecular details about how piRNAs put genes on lock-down. Because RNA is genetic material, it can match up to specific sequences of DNA letters. A cell may contain hundreds of thousands of piRNAs, each with a unique combination of 24 to 32 RNA units, or nucleotides, says Haifan Lin, a stem cell biologist at Yale University. The piRNA’s sequence is like an address on a letter specifying where a protein called Piwi should recruit proteins that make epigenetic modifications, Lin and colleagues reported in the March 11 Developmental Cell. In the fruit flies Lin studies, as in worms, the modifier proteins stick methyl groups onto histones. But Lin thinks piRNAs may similarly direct DNA methylation enzymes in mammals, including humans.
Miska is impressed, and a bit troubled, that piRNAs seem to place a vise grip on genes. “This is something that is amazing, but I also find it very scary,” he says.
Scary because epigenetic marks were long assumed to be malleable and respond to the environment. If the epigenetic programming gets stuck, an organism may find itself ill-adapted to the world around it. Some evidence suggests that addiction and mental illnesses may result (SN: 5/24/08, p. 14).
So far, Miska’s team has not found a way to reverse piRNAs’ grip. But the worms in his experiment are inbred. He thinks that mating with unrelated worms might help release the hold. Even in inbred worms, 20 to 40 percent of offspring can “forget” their epigenetic immunity to viruses. “There is a way out, which I find very comforting,” Miska says.
If there really is a way out for the worms, it could mean that animals and people operating in a more natural environment have already discovered the escape hatch: mating with someone with different piRNAs.
No one knows how piRNAs might determine which epigenetic burdens trickle down through the generations. Even more is still unknown about what inherited epigenetic changes may mean for human health. Although lab experiments paint a rather worrisome picture, scientists emphasize that epigenetics may also cement positive changes. Even if your great-grandparents didn’t have the healthiest of habits, following public health advice about exercising and eating a healthy diet may program beneficial epigenetic changes that are good for you and future generations.