‘In the Blood’ traces how a lifesaving product almost didn’t make it
The book explores the tumultuous history of a blood-clotting invention
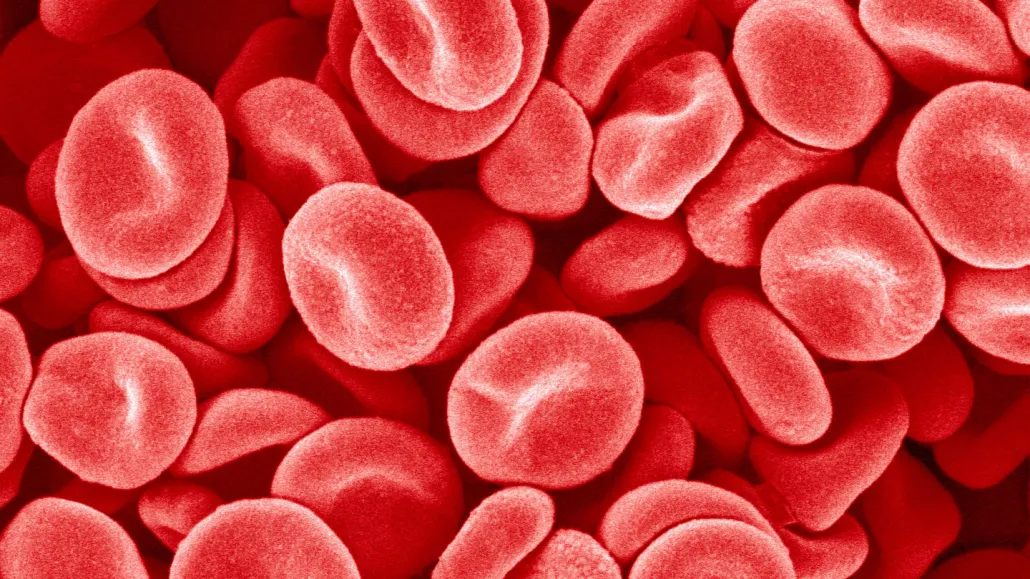
Scientists have been working for years on products to help stanch blood loss (red blood cells shown). One such invention, called QuikClot, speeds up the clotting process by drawing water from blood.
Micro Discovery/Corbis Documentary/Getty Images
In the Blood
Charles Barber
Grand Central Publishing, $29
The average human body holds about 5 liters of blood. Lose a liter, and you may go into shock. Lose two more, and you’ll probably die.
For doctors treating traumatic injuries, keeping a patient’s blood in their body is “one of the most fundamental problems of survival,” Charles Barber writes in his fast-paced new book, In the Blood.
Solutions to that problem haven’t changed all that much in centuries. Doctors can pack a wound with gauze or put pressure on blood vessels to slow bleeding. While other areas of medicine have leaped ahead over time, Barber notes, emergency medicine has largely stood still, an inertia that’s had deadly consequences. Some 50,000 people in the United States bleed to death every year.
You’d think, then, that a product that can stanch bleeding would be celebrated in the streets, snapped up immediately by military doctors and emergency rooms alike. You’d be wrong. In the Blood chronicles the invention and bafflingly slow adoption of QuikClot and its successors, inexpensive clotting agents that can stop big bleeds in minutes. Barber, who’s also written about criminal justice and mental health, leads readers on the path from product invention to implementation — and it’s a treacherous journey.
Barber starts his story, which races like a thriller, in Mogadishu, Somalia, at the scene of the 1993 battle that inspired the movie Black Hawk Down. After two American helicopters were shot down, John Holcomb, then a U.S. Army major, and other doctors treated dozens of injured soldiers, many of whom died from loss of blood.
That horrific experience electrified Holcomb. Better hemorrhage control was urgently needed, and he was the man to lead the charge. In 2002, Holcomb became head of the Army Institute of Surgical Research, a research laboratory focused on improving combat casualty care. Holcomb championed the development of different clotting candidates, including HemCon, a bandage containing a shrimp-shell chemical, and Factor Seven, an injected drug that boosts the body’s clotting capability, sometimes lethally, it turned out.
In Barber’s telling of the story, Holcomb’s character is complex, shifting between savior and villain. Under his watch, the Army poured millions of dollars into his favorite products. It’s hard to grasp what motivated Holcomb, but Barber argues that he was long unwilling to consider other options — like QuikClot — data be damned. QuikClot seemed to be more effective than the rest. But it didn’t come with a big Army budget or a biotech company’s backing. It was born in an inventor’s basement.
The inventor was Frank Hursey, a mild-mannered engineer from Connecticut who discovered in 1983 that the ground-up mineral zeolite could mop up the water in blood. By concentrating the molecules involved in clotting, Hursey’s invention sped up the process. In 1999, he partnered with “swashbuckling salesman” Bart Gullong, who helped develop and promote the product. Barber pulls readers into their adventure, though he occasionally meanders too far into their backstories.
The action picks up when Barber digs into the evidence behind different clotting agents. He describes clear-cut animal tests, moving accounts from soldiers in the field and reports linking Factor Seven to stroke, heart attack and death. A central question of the book, then, is not so much “How do you stop a hemorrhage?” as “How do you get a hemorrhage-stopping product to the people who need it?”
Hursey and Gullong were up against entrenched military and pharmaceutical interests from the get-go. The company that produced Factor Seven aggressively marketed the drug, Barber reveals, even in the face of its flaws. It’s clear that he is rooting for the underdogs. He lays out facts for readers like a mason placing bricks, building a solid case against a system where money sways whether a medical product gets used. Even when the data suggest it shouldn’t.
In 2008, Holcomb finally recommended an improved version of Hursey’s invention, called QuikClot Combat Gauze, for use in the military, “an almost unimaginable victory,” Barber writes. In recent years, QuikClot gauze has made its way into hospitals, and consumers can now buy it on Amazon for $18.99.
Though Hursey remains largely unknown, Barber calls his discovery “paradigm-shifting.” Hursey “took bleeding control largely out of the hands of doctors,” Barber writes, “and put it into the hands of police officers, EMTs, adventurers, soldiers, hikers, and moms and dads.”
Buy In the Blood from Bookshop.org. Science News is a Bookshop.org affiliate and will earn a commission on purchases made from links in this article.







