Researchers have found a new way to make a temporary chink in the brain’s armor, opening the door for treatments to get in. The results of a rodent study, published September 14 in the Journal of Neuroscience, may highlight a method to sneak therapies for diseases such as Alzheimer’s, HIV and cancer past the blood-brain barrier.
“It’s a very interesting development,” says Celia Brosnan of the Albert Einstein College of Medicine in the Bronx, N.Y. “It has considerable potential, but obviously there’s a lot that needs to be followed up on.”
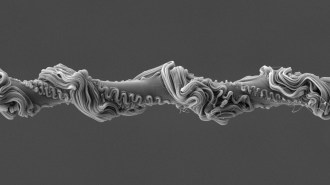
Many potentially useful compounds exist to treat neurological diseases, notes study coauthor Margaret Bynoe of Cornell University College of Veterinary Medicine in Ithaca, N.Y. “The problem is getting them into the brain,” she says, where walls of specialized cells line blood vessels and keep harmful substances out. Since this barrier also impedes drugs, researchers have been eager to find a safe and effective way to get past it.
In the new study, Bynoe and colleagues targeted molecules that sit on the surface of blood-brain barrier cells. Using a compound called NECA to activate these molecules, called adenosine receptors, in mice caused the barrier to open for up to 18 hours, the team found. After this activation, bulky sugar molecules introduced by the researchers, along with giant antibodies engineered to scoop up the Alzheimer’s-related protein amyloid-beta, crossed from the blood into the brain.
Next, the researchers tested another substance that activates adenosine receptors — a compound called Lexiscan, which is approved by the U.S. Food and Drug Administration for use in heart imaging. Five minutes after a single injection of Lexiscan, the big sugar molecules showed up in the rodents’ brains. Three hours later, the blood-brain barrier was back to normal, the scientists reported.
The transience of such a window is important, says Brosnan. Therapies that permanently damage the brain’s protective shield or leave it open for a long time raise the risk of damage. “After all, the blood-brain barrier is there for a very good reason,” she says.
An effective way to get drugs into the brain could have an enormous impact on diseases such as Alzheimer’s, Parkinson’s and brain cancers and on viruses such as HIV and herpes, says Bynoe. Antiviral drugs keep HIV replication in check in the body, but the virus can safely hide in the brain, she says. “When you think of the millions of people that are infected with HIV, the potential of being able to eradicate this virus by being able to get anti-HIV medication into the brain is phenomenal.”
Although the new results might offer a viable way to sneak medicines past the blood-brain barrier, such an approach would need to be thoroughly tested for each disease and drug, says pharmaceutical scientist Alexander Kabanov of the University of Nebraska Medical Center in Omaha. “There’s a long road from here to clinical applications.”