Preeclampsia, a life-threatening condition that strikes during pregnancy, may have a lot in common with Alzheimer’s and mad cow diseases, a new study suggests.
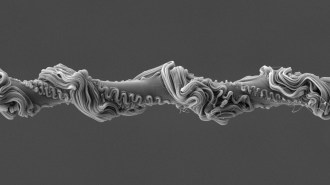
Misfolded proteins, including one involved in Alzheimer’s, clump in the urine of women with preeclampsia, researchers report in the July 16 Science Translational Medicine. Those twisted proteins are produced by the placenta, a pancake-shaped organ that fuses to the uterine wall and nourishes the fetus.
A urine test could detect the abnormal proteins up to 10 weeks before symptoms began, say Irina Buhimschi, an obstetrician at Nationwide Children’s Hospital in Columbus, Ohio, and colleagues.
Preeclampsia is a complication of pregnancy that results from a damaged placenta and raises women’s blood pressure to dangerously high levels. It affects about 5 to 10 percent of pregnancies. Along with other high blood pressure disorders of pregnancy, preeclampsia kills about 76,000 women and 500,000 babies worldwide each year. It usually occurs after 20 weeks of gestation. There is no treatment except delivering the baby and the placenta.
Buhimschi and her colleagues examined the urine of women with preeclampsia and found that at least five proteins routinely aggregate when the researchers added a dye called Congo red. The dye is known to glom onto proteins that contort into fiber-forming shapes called amyloids. Amyloid proteins have been implicated in many diseases, including Alzheimer’s, Parkinson’s and mad cow disease.
Among the clumpy proteins Buhimschi and her colleagues discovered in the urine was amyloid precursor protein, or APP, a protein that, when cleaved into fragments, forms plaques in the brains of people with Alzheimer’s.
The five amyloid proteins were also found in the placentas of women with preeclampsia. Exactly what the proteins are doing there is not clear. They may damage the placenta and cause preeclampsia or may be a side effect of the disease, researchers say.
Placentas and brains make many of the same proteins, so it’s not so surprising to find a brain protein like APP in the placenta, says Susan Fisher, a human reproductive and developmental biologist at the University of California, San Francisco. Researchers now need to figure out whether the amyloid proteins are damaging the placenta, she says.
Many pregnancy complications including preeclampsia are accompanied by a buildup of proteins between the placenta and the uterus. No one knows whether amyloid proteins are part of the protein layer and whether they occur only in preeclampsia, Fisher says.
The discovery could help researchers studying disorders other than preeclampsia. Researchers may learn more about the biology of protein-misfolding diseases from studying a fast-moving condition such as preeclampsia, rather than diseases that take decades to develop, says Thomas Easterling, a maternal-fetal medicine specialist at the University of Washington in Seattle.
The research may also be of value for detecting the disease early in pregnancy, Easterling and other researchers say. Currently, doctors have little warning that the disease is about to hit. That leaves almost no time to attempt to correct the condition, says John Kingdom, a maternal-fetal medicine specialist who directs a placenta clinic at Mount Sinai Hospital in Toronto.
If the new test proves a reliable early indicator, it would leave “a big wide window between detection and symptom onset” in which doctors could take action, he says. That could give experimental treatments a betters shot at success.
Because the test uses urine instead of blood, it would be cheap and easy. It could even be done at home, Kingdom says. That would make it attractive in developing countries, where most of the deaths from the disease occur, he adds.
But there is a long way to go before this test is used clinically, says Bahaeddine Sibai, a maternal-fetal medicine specialist at the University of Texas Health Science Center at Houston. In the last decade or so, many researchers have claimed to have discovered substances that could predict preeclampsia before symptoms began. None have panned out, Sibai says.
He worries that the urine test might falsely predict that a woman will develop preeclampsia. Only a small number will actually be affected. “The rest you’ll scare the heck out of,” he says.
Exactly what action doctors could take to correct the disease if detected early isn’t known, and many potential treatments could even worsen health. Bringing down a mother’s high blood pressure could choke off blood and oxygen flowing to the fetus, Sibai says. And even if researchers had a way to break up amyloid clumps in women with preeclampsia, the treatment might not make the condition better, he says.
The way to deal with preeclampsia remains elusive, says Sibai. “You have to find something that will repair the injury to the placenta.”