Prescription for Controversy
Medications for depressed kids spark scientific dispute
Among medications, antidepressants take the prize for inciting public and media mood swings. Whether celebrated as depression-busting happy pills or dismissed as overrated and apt to cause dangerous side effects, selective serotonin reuptake inhibitors (SSRIs) have taken pharmaceutical firms on a financial joy ride. Since their U.S. introduction in 1989, they’ve become the best-selling medication of any kind, reaping an estimated $10 billion annually in worldwide sales. Roughly one adult in eight has tried an SSRI in the past decade.
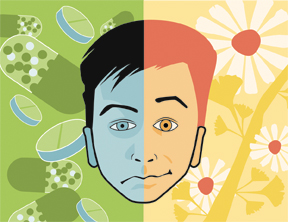


The seven currently marketed SSRIs are frequently prescribed to people diagnosed with major depression or with anxiety ailments such as obsessive-compulsive disorder or social phobia. Increasing numbers of depressed children and teenagers take SSRIs. Use of antidepressants among youngsters ages 5 to 17 increased from about 2 percent of that population in 1994 to almost 6 percent in 2002. This rapid expansion has served up a heavy dose of scientific debate mixed with regulatory scrutiny.
U.S. and British regulatory agencies approved one SSRI, fluoxetine (Prozac), for children and adolescents in 2003. The next year, however, the Food and Drug Administration responded to concerns that SSRIs cause youngsters to contemplate suicide or to kill themselves. The agency reviewed 24 studies of children and teens with major depression or other psychiatric disorders treated for 1 to 4 months either with one of nine antidepressant drugs, including SSRIs, or placebo pills.
On average, across the reviewed studies, 4 percent of patients taking antidepressants—mostly SSRIs—reported suicidal thoughts or acts compared with 2 percent of those taking placebos. Yet weekly questionnaires filled out by patients in 17 studies indicated that medication neither inflamed longstanding suicidal tendencies nor created them in people who had never considered killing themselves. Reasons for the discrepancy are unclear.
In March 2004, FDA officials issued a label for antidepressant containers warning that the medications may prompt young people to contemplate and try to commit suicide. Around the same time, a medical commission England tightened guidelines for using SSRIs and other antidepressants in adults, recommending the drugs only for the initial treatment of moderate-to-severe depression, preferably in combination with psychotherapy.
These developments reflect growing public concern with potential side effects of SSRIs and the way such drugs are tested and regulated, says psychiatrist Klaus P. Ebmeier of the University of Edinburgh in Scotland.
Some researchers doubt that SSRIs work as well as many psychiatrists and pharmaceutical firms claim they do. “The data for antidepressants’ efficacy over and above that of placebos are not so compelling,” says neuroscientist Amir Raz of Columbia University in New York City. No one knows the long-term effects of these drugs on developing brains, he adds.
Given the potentially fatal consequences of leaving depression untreated, many psychiatrists regard mounting worries about SSRIs as excessive. “Public fears that drug treatment for depression is worse than the illness itself may lead to untreated depression and more suicide,” says Darrell A. Regier, director of research for the American Psychiatric Association in Washington, D.C.
All that controversy swirls around a towering problem. An estimated 1.5 million 12- to 18-year-olds in the United States, roughly 2 percent of that age group, experience major depression. That total dwarfs the number of mental-health clinicians qualified to treat them. Only around 7,000 psychiatrists in this country have been trained to treat children and adolescents.
Drug patrol
Reports of adults whose suicidal thoughts and behaviors emerged or worsened during SSRI treatment began to appear in medical journals in 1990. A medical task force assembled by the American College of Neuropsychopharmacology (ACNP) examined those reports in 1993. It concluded that the available scientific evidence raised no red flags about SSRIs’ promoting or causing suicide but added that clinicians should monitor drug-treated suicidal patients closely.
A second ACNP task force has now conducted a follow-up review and reached similar conclusions for depressed children and adolescents. Its findings appear in the March Neuropsychopharmacology. After analyzing British and U.S. clinical studies that relied on questionnaires, the task force noted that individuals prescribed SSRIs reported slightly more instances of suicidal thinking and suicide attempts than placebo-treated peers did. But these figures varied considerably from one trial to another, suggesting that the questionnaires inaccurately measured suicidal tendencies, says psychiatrist and task force chair J. John Mann of Columbia University.
Other lines of evidence cited by Mann and his colleagues suggest that SSRIs don’t foster suicide and may instead prevent it. For example, a dramatic increase in the number of SSRI prescriptions for teens over the past 15 years coincided with an average decline of 33 percent in youth-suicide rates in the United States and 14 other countries.
Also, studies of teens and adults who have killed themselves—including an analysis of nearly 15,000 suicides in Sweden—rarely find traces of SSRIs or other antidepressants in blood, even among those who were depressed.
Suicidal thoughts and attempts in depressed children and adolescents escalate in the month before starting SSRI treatment and progressively decline in the 6 months after initiating SSRI use, say psychiatrist Gregory E. Simon of Group Health Cooperative in Seattle and his colleagues. Their study, considered by Mann and his colleagues before its publication, appeared in the January American Journal of Psychiatry.
Simon’s team identified 82,285 episodes of treatment with SSRIs or any of several other antidepressant drugs among 65,103 health-plan members. Patients age 17 years or younger accounted for 5,107 treatment episodes, each of which was tracked by the researchers for 6 months. Treatment occurred between 1992 and 2003.
Overall, 31 people of any age killed themselves—a far lower proportion of depressed patients than occurs without antidepressant treatment—and 76 made suicide attempts that landed them in the hospital.
Among the cases examined, attempted suicide occurred more often among teens than among adults in the month before starting treatment. In both age groups, the rates of completed and attempted suicides were about 60 percent lower during antidepressant treatment.
Still, large studies using random assignment to various SSRIs or a placebo are needed to establish whether particular drugs cause suicide attempts in certain patients, Simon says.
One such study compared 439 depressed youngsters assigned to receive Prozac or a placebo with or without 4 months of cognitive-behavioral therapy, a form of psychotherapy that focuses on reversing negative thinking and setting new goals (SN: 8/21/04, p. 116: Available to subscribers at Lifting the Mood: Depressed teens benefit from combined therapy). The test found that, for moderate-to-severe depression, many youngsters improved markedly with a combination of Prozac and psychotherapy, and Prozac alone worked nearly as well.
In this investigation, dubbed the Treatment for Adolescents with Depression Study (TADS), rates of suicidal thoughts dropped in all four groups, although only the combination of Prozac and psychotherapy proved superior to placebos in this respect.
These studies remain incomplete. Drug companies have yet to release unpublished data from some clinical trials requested by the ACNP task force, Regier notes. Political pressure is building to require the release of unpublished results.
Placebo power
One major theme emerging from studies of depression treatment, according to Raz, is that SSRIs and related medications relieve depression only slightly better than placebo pills do. For example, the ACNP task force recommends Prozac as a depression treatment in youth because it showed statistical superiority to placebo pills in 3 of 15 clinical trials. No other SSRI or older antidepressant outperformed placebos in more than one of the clinical trials that the group examined.
The TADS study was more encouraging. Many of the depressed teens improved markedly with a combination of Prozac and cognitive-behavioral therapy or Prozac alone. Fewer responded to the psychotherapy alone or to placebo pills.
Yet many studies of drug treatment for depressed children and teenagers show small, if any, benefits of SSRIs over placebos, Raz concludes in a research review published in the January PLoS Medicine.
Psychologist David O. Antonuccio of the University of Nevada School of Medicine in Reno also stresses placebo power. In a 2004 analysis of nine clinical trials of SSRIs and other antidepressants prescribed to depressed youngsters, he and psychologist Irving Kirsch of the University of Plymouth, England, concluded that placebos worked 88 percent as well as active medication did.
A second analysis conducted by Kirsch and psychiatrist Joanna Moncrieff of University College, London, found that placebos achieved 80 percent of the antidepressant response observed in adults. That investigation was reported in the July 16, 2005 British Medical Journal.
These two studies have generated controversy in psychiatric circles. Psychiatrist Michael E. Thase of the University of Pittsburgh Medical Center and others argue that antidepressants’ narrow margin of superiority over placebos often translates into substantial gains in daily functioning for those with moderate-to-severe depression, especially as treatment extends beyond the few months allotted for clinical trials. Thase also points out that the TADS results illustrate the clout of combining SSRIs with psychotherapy.
Raz responds that volunteers in the TADS investigation knew whether or not they were getting psychotherapy. Depressed teens may have expected to feel better when given a treatment that they knew was genuine, he proposes.
Furthermore, Raz contends that the drugs’ superiority, assessed in the various studies by using a standard rating scale of depression symptoms, may qualify as statistically significant even when that advantage doesn’t translate into significant improvements in a person’s daily functioning. The absence of clear criteria for identifying life-changing upgrades in mood and behavior generates scientific confusion, in his view.
There’s little information available about the long-term effects of SSRIs. Animal studies suggest that serotonin, the neurotransmitter targeted by SSRIs, assists in early brain development, especially in areas involved in anxiety responses. Mouse studies indicate that exposure to Prozac in infancy leads to excessive fear and anxiety in adulthood.
It’s far from clear precisely how SSRIs act in the brain, Raz adds. Although the drugs reduce serotonin’s availability for performing its various duties, that effect can influence the activity of other neurotransmitters.
Only more studies over many years will determine whether youngsters prescribed SSRIs develop an increased vulnerability to anxiety disorders later in life, Raz says.
There’s no guarantee, however, that future investigations will settle this issue. The pharmaceutical industry’s vast influence on biomedical research includes its funding of clinical trials of SSRIs and financial support for most psychiatric researchers via grants, speaking fees, and consulting arrangements. Consider that, at the end of the group’s report, 10 of 11 members of the ACNP task force list financial ties to pharmaceutical firms.
This influence will probably continue to emphasize positive over negative results, in Raz’s view. For example, a team led by psychologist Craig J. Whittington combined data from published and unpublished clinical trials of five SSRIs prescribed to depressed children and adolescents. The group obtained the unpublished data from government regulators in England.
Taken together, the findings indicated that only Prozac outperformed placebos and that participants taking the placebos and Prozac had slightly lower rates of suicidal thoughts and attempts than those taking other SSRIs had. However, the researchers reported in 2004, the unpublished reports presented a less favorable view of the drugs’ actions than the published work did. This raises the disturbing possibility that pharmaceutical companies have held back data that reflect poorly on their drugs, Raz says.
“The placebo effect can teach us a great deal about how to tailor depression treatments to those individuals who are placebo responders,” he says. Approaches such as exercise and diet should be examined as possible alternatives for these people, Raz suggests.
In the trenches
As conflict rages over SSRI treatment for depressed kids, clinicians face hard choices about how to assist young people in emotional turmoil.
Psychiatrist Leon Hoffman directs the Pacella Parent Child Center in New York City. “In my experience, depressed kids often get better with psychotherapy alone,” Hoffman says. “If a child is suicidal, I’ll think about prescribing medication.”
A new review of 35 studies of youth-depression treatments that didn’t include drugs indicates that various psychotherapies yield substantial improvement, compared with relaxation training or other placebolike regimens. These effects last for several months after psychotherapy ends but then fade quickly, conclude psychologist John R. Weisz of Judge Baker Children’s Center in Boston and his coworkers in the January Psychological Bulletin.
Antonuccio is concerned that harried physicians write prescriptions for SSRIs without talking in depth to emotionally troubled young patients.
Inaccurate diagnosis of depression complicates treatment, Hoffman adds. Clinicians need to ensure that depressed children don’t actually suffer from bipolar disorder with its alternating periods of depression and mania, a phase characterized by euphoria and impulsive behavior.
Antidepressants can make such youngsters agitated, volatile, and possibly suicidal. At the same time, the number of diagnoses of childhood bipolar disorder has gone up so rapidly in the past few years that Hoffman suspects that some kids are being inappropriately tagged with this condition.
Even in children who clearly exhibit major depression, clinicians need to rein in any expectations that SSRIs automatically transform lives in a consistent way, Hoffman adds. “Antidepressants don’t work like magic,” he remarks.