Scientists probe Zika’s link to neurological disorder
Uptick in cases of Guillain-Barré syndrome raises concern among health officials

SUDDEN PARALYSIS Patients with Guillain-Barré syndrome can experience facial paralysis, like this patient (right) at a hospital in Colombia. The country has seen an uptick in cases of the neurological disorder, which scientists have linked to Zika virus infection.
AP Photo/Ricardo Mazalan
For some adults, Zika virus is a rashy, flulike nuisance. But in a handful of people, the virus may trigger a severe neurological disease.
About one in 4,000 people infected by Zika in French Polynesia in 2013 and 2014 got a rare autoimmune disease called Guillain-Barré syndrome, researchers estimate in a study published online February 29 in the Lancet. Of 42 people diagnosed with Guillain-Barré in that outbreak, all had antibodies that signaled a Zika infection. Most also had recent symptoms of the infection. In a control group of hospital patients who did not have Guillain-Barré, researchers saw signs of Zika less frequently: Just 54 out of 98 patients tested showed signs of the virus.
The message from this earlier Zika outbreak is that countries in the throes of Zika today “need to be prepared to have adequate intensive care beds capacity to manage patients with Guillain-Barré syndrome,” writes study coauthor Arnaud Fontanet of the Pasteur Institute in Paris and colleagues, some of whom are from French Polynesia.
The study, says public health researcher Ernesto Marques of the University of Pittsburgh, “tells us what I think a lot of people already thought: that Zika can cause Guillain-Barré syndrome.” As with Zika and the birth defect microcephaly (SN: 2/20/16, p. 16), though, more work needs to be done to definitively prove the link.
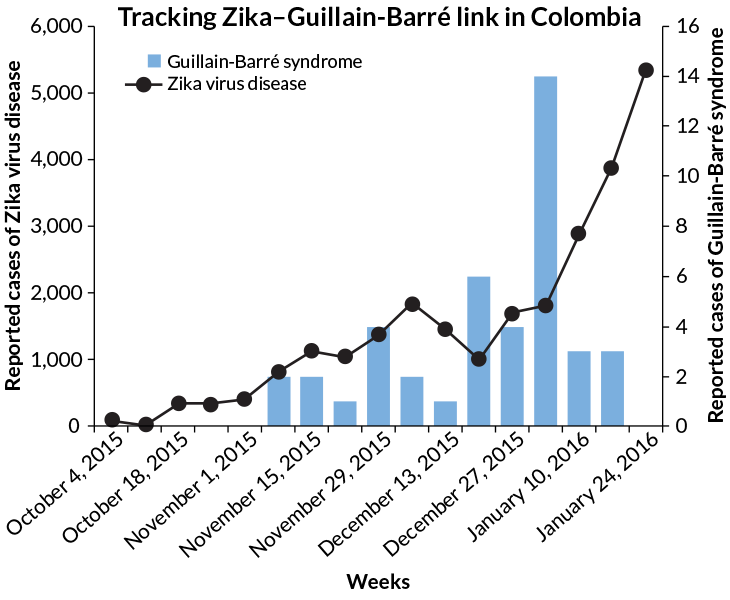
Several countries currently hard-hit by Zika have reported upticks in Guillain-Barré syndrome. Colombia, for instance, usually sees about 220 cases of the syndrome a year. But in just five weeks between mid-December 2015 to late January 2016, doctors diagnosed 86 cases, the World Health Organization reports. Other Zika-affected countries, including Brazil, El Salvador and Venezuela, have also reported unusually high numbers of cases.
Despite the seemingly strong link between Zika and Guillain-Barré, Marques stresses that the risk of getting the syndrome after a Zika infection is quite low. “It’s important that people don’t think that if you get Zika, you are going to get Guillain-Barré.” The chance is much less than 1 percent, he says.
And it’s too early to say whether the rate of Guillain-Barré estimated in the paper will be the same in ongoing Zika outbreaks, says Anna Durbin, a vaccine researcher at Johns Hopkins University. “We have a number now, but it’s not perfect,” she says. Ongoing studies in Brazil and other countries affected by Zika will help refine the rate.
Story continues after graph
The syndrome begins as the body’s immune system attacks peripheral nerves, causing weakness or tingling sensations in the lower extremities. In severe cases, total paralysis can result, leaving people dependent on ventilators in intensive care units while they recover. Three to 5 percent of people with Guillain-Barré die from complications, scientists estimate.
Other viruses, including HIV, influenza and dengue (like Zika, a flavivirus), are known to spark Guillain-Barré, possibly through their interactions with the body’s immune system, though the details remain mysterious.
The timing of Guillain-Barré’s onset may make it easier for scientists to pin the disorder on Zika. Because the syndrome shows up days or weeks after an infection subsides, Guillain-Barré may offer a quicker readout of Zika’s effects than waiting months to see if microcephaly in babies are born to infected mothers, the WHO’s Bruce Aylward said in a news briefing February 19.
Scientists conducting a multinational Guillain-Barré study may soon expand their study, called the International Guillain-Barre Syndrome Outcome Study, into Brazil and Colombia to look for signs of Zika infection in people with the syndrome. “We are developing a new version of the IGOS protocol that is more focused on Zika and other flaviviruses, to support the research in those countries,” says Bart Jacobs, an immunologist at Erasmus University Medical Center in Rotterdam, the Netherlands, who’s helping supervise the study. Further studies could also help explain why some people are susceptible to Guillain-Barré. Genetics, previous viral infections or toxins may all play a role.