Study clarifies obesity-infertility link
Effect of insulin in pituitary surprises scientists
Being obese has long been linked to infertility in females, but researchers may have been wrong about how the link was forged, a new study suggests.
Doctors and scientists have thought that the fertility problems were caused by resistance to the hormone insulin. Chronically high levels of insulin often accompany obesity, eventually making muscles and other tissues impervious to the hormone’s signals.
A new study in mice shows that the pituitary gland, which helps regulate the release of fertility-associated hormones, remains sensitive to insulin. But in obese mice, insulin’s constant signaling to release the fertility hormones leads to an overabundance of those hormones, and consequently infertility, researchers report in the Sept. 8 Cell Metabolism.
The discovery firmly ties metabolism to fertility in an unexpected way and may have implications for treating women with a condition known as polycystic ovary syndrome, which is characterized by abnormal menstrual cycles and is often associated with obesity and type 2 diabetes.
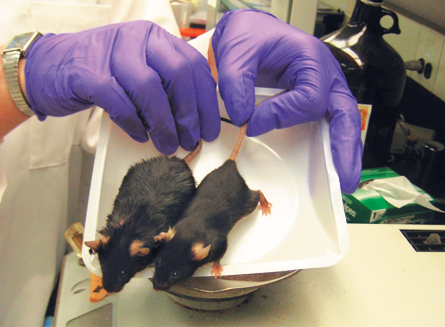
Researchers led by Andrew Wolfe of Johns Hopkins University stumbled upon the discovery when studying mice genetically engineered to lack proteins called insulin receptors that sit on the surface of a cell, latch onto insulin and pass along the hormone’s message to the rest of the cell. The team had engineered the mice so that insulin receptors were missing only from cells in the pituitary, a gland that it is important for regulating many important body functions, including fertility.
Female mice fed a high-fat diet become obese and have a hard time reproducing. But, to the researchers’ surprise, fat females lacking insulin receptors in their pituitary glands remained fertile. The result was unexpected because researchers had thought that removing insulin receptors would have the same effect as had been theorized in obesity – making the pituitary impervious to insulin signals, and thus less able to release two hormones that help regulate ovulation and fertility.
Instead, the team discovered that the pituitary does not lose its ability to respond to insulin. As insulin levels rise with weight gain, the pituitary releases ever higher levels of the fertility-regulating luteinizing hormone. Chronically high levels of luteinizing hormone and other signals released by the pituitary disrupt the natural cycle of fertility hormones that signal the ovaries to release eggs.
“If you disrupt the hormone levels and the timing, it’s very easy to disrupt fertility in females,” Wolfe says. Removing the insulin receptors in the pituitary keeps the gland from going into overdrive and releasing too much of the fertility hormones in the obese mice.
The new study “ushers in a new era of thinking” about the link between fertility and metabolism, says Gary Hausman, a physiologist at the U.S. Department of Agriculture’s Agricultural Research Service in Athens, Ga.
“I just didn’t think that insulin could be such a big role-player, especially in the pituitary,” Hausman says. But the evidence presented in the new study “is so clear, it’s so blatant, that I really have to think more about this.”
Insulin seems to be helping the pituitary monitor the availability of food and other conditions necessary for the survival of offspring, but it is not clear whether insulin would have the same effect on the pituitary in people as it does in mice, says Mark Lawson, a reproductive biologist at the University of California, San Diego. In people, levels of luteinizing hormone go down with rising body weight, not up. But Lawson says insulin may have other effects on the brain and the ovaries, two important organs affecting fertility.
The study nevertheless shows that an energy sensor such as insulin can have a direct effect on reproduction and may give new insights into how infertility may be treated in the future, Lawson says.
“We have to pay attention to the direct action of insulin on the reproductive tract,” he says.







