The United States was on course to eliminate syphilis. Now it’s surging
The syphilis crisis is hitting pregnant people and newborns especially hard
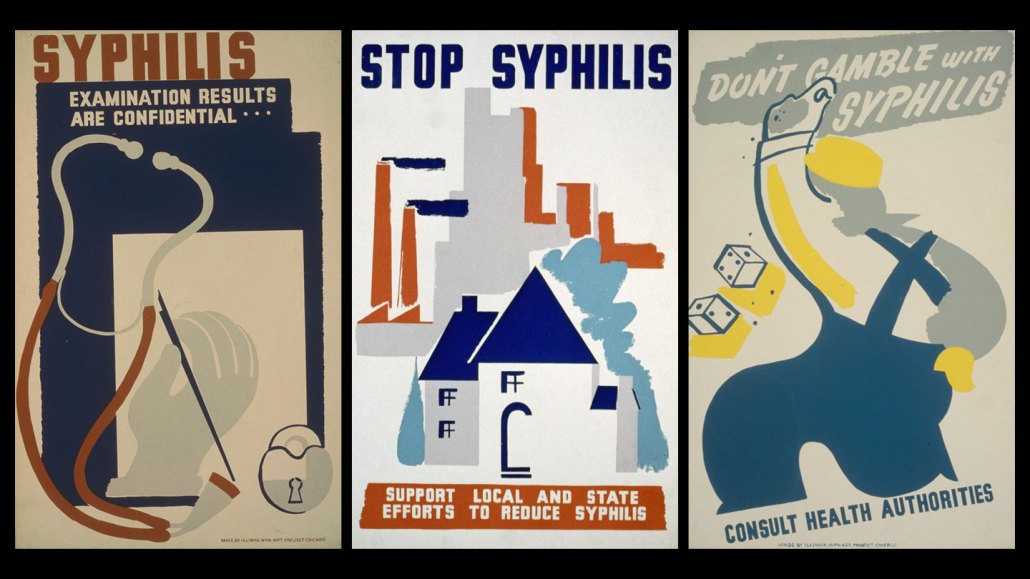
These public health posters, made as part of the Federal Art Project, encouraged syphilis screening during the Great Depression. National data collection for syphilis began in 1941. The rate in the 1940’s was as high as 450 cases per 100,000 people.
Illinois WPA Art Project
Once on the path to eliminating syphilis, the United States has reversed course, with cases of the infectious disease surging.
From a low of under 32,000 cases in 2000, the number of people with syphilis has rocketed to more than 207,000 in 2022, the U.S. Centers for Disease Control and Prevention reported in January. That’s 62 cases per 100,000 people.
The crisis is hitting pregnant people and babies especially hard. The maternal rate for syphilis during pregnancy rose from 87 per 100,000 births in 2016 to 280 per 100,000 births in 2022, the CDC reported on February 13. Without treatment, pregnant people can pass a syphilis infection to the fetus. That can cause congenital syphilis and lead to miscarriage, stillbirth, premature birth, severe health problems after birth or the infant’s death. More than 3,700 babies were born with syphilis in 2022, roughly ten times the number in 2012.
Testing is a crucial step in finding cases. Syphilis is “the great pretender,” says Allison Agwu, a pediatric and adult infectious disease clinician and researcher at Johns Hopkins School of Medicine. “It can look like a bunch of other things.” The disease moves through several stages, at times featuring symptoms common to other conditions and at other times having no symptoms.
People can get tested — usually with a blood test — by their primary care provider or at a public health clinic or an urgent care facility, for example. With syphilis rates so high, Agwu would like to see testing for syphilis destigmatized and become easier to discuss as part of a regular medical checkup. “If you have been sexually active ever, you should have a syphilis test,” she says.
Science News spoke with Agwu about the surge in cases and what needs to be done better to prevent syphilis. The interview was edited for length and clarity.
SN: What are some of the factors behind the rise in syphilis cases in the United States?
Agwu: It’s multifactorial. Syphilis is oftentimes asymptomatic, so people can have it for years and not know they have it — they missed the signs when it was symptomatic. We have a whole public health infrastructure imploding with decreased access and funding. The impact is magnified in communities that have the least access to begin with and that are relying on those clinics or places that funding is being pulled from. There is stigma. There have been medicine shortages.
The infrastructure [built] to control syphilis — almost eliminating the disease a few decades ago — has really collapsed. We’re at this perfect storm for increases in syphilis and, as a result, congenital syphilis as well.
SN: Where are there missed opportunities in testing for syphilis?
Agwu: I’ve been in the infectious disease field for a long time. We’ve had the 80-year woman who comes in and she’s confused or disoriented. That’s neurosyphilis [a complication of syphilis that impacts the brain and nervous system], from never being treated for a syphilis infection. We all should be thinking about syphilis, particularly with the rates that we’re seeing. Healthcare providers should just test people.
There’s testing in early pregnancy. If someone is diagnosed with syphilis, they should be treated in pregnancy. This is one of the times you absolutely need to treat them to avert transmission to the baby. I think part of the challenge with syphilis in pregnancy — actually, all sexually transmitted infections in pregnancy — is that oftentimes there are people that society thinks of as sexual beings and those that we do not. I’ve talked to pregnant women who say, well I got my testing, but there was not a conversation about how I can stay negative. So the counseling around staying negative, I think we may miss that.
We certainly have had scenarios where the baby comes, and the mom or the birthing parent has had no prenatal care. [In that case] we’re testing at delivery.
Rising maternal syphilis rates
The maternal syphilis rate, the number of live births to women with syphilis per 100,000 live births, increased for all groups from 2016 to 2022. The biggest jump — 783 percent — occurred among American Indian and Alaska Native women giving birth.
SN: What needs to happen to bring syphilis cases back down?
Agwu: It’s education, and not in a way to scare people, but just: This is what you can have and the different ways you can get it, and here’s how you can test for it, here’s where you can test for it.
We need to normalize sexuality and sexual exploration and not vilify it. We need to destigmatize the diagnosis so people are more likely to then tell their partners, so their partners can also get tested and treated. Instead of having someone prove that they need to have additional testing, how about we just test people — instead of creating a stigma around, well do you need to get tested again. Acknowledging that people are sexual beings, even when they’re pregnant.
COVID-19 really highlighted the problems we were having with our public health infrastructure. We need to think about how we can effectively provide sexual health care and give testing, prevention, treatment all in a way that is packaged in a positive light. Take it out of the dark.
The stages, testing and treatment of syphilis
Syphilis — caused by the bacteria Treponema pallidum — is described in terms of stages.
In the first stage, the only sign is one or several sores at the site a person was infected, such as on the penis, around the vagina, in the anus or mouth. The sores are usually painless and remain for three to six weeks. During the second stage, people can have a rash, headaches, fever, muscle aches or fatigue.
Once those symptoms pass, a person can be asymptomatic for years. But some people progress to a fourth, potentially fatal stage, which damages many organs, including the brain, nerves and heart.
The guideline for asymptomatic adolescents and adults is to test those who have been sexually active and are at increased risk, which includes people who have an HIV infection or other sexually transmitted infections and men who have sex with men. The recommendation for pregnant people is to test for syphilis as early as possible, ideally during their first prenatal visit.
Syphilis is treated with a shot of a special formulation of penicillin. There has been a shortage of the drug, which is the only effective treatment during pregnancy. Nonpregnant people can also take the oral antibiotic doxycycline for treatment.







