Against the Migraine
A procedure's serendipitous success hints that some headaches start in the heart
Neurologist Roman Sztajzel received an unexpected letter in 1999 from a patient he had last seen a year and a half earlier. The Swiss woman thanked him for curing her of migraines, which she had experienced frequently into her early 30s. But Sztajzel hadn’t treated her for migraines. He’d seen her because she’d had a stroke. Another stroke soon followed. Neither brain attack showed any sign of a typical cause. In search of an explanation, Sztajzel and his colleagues had screened the woman for an abnormal opening between the heart’s upper chambers.
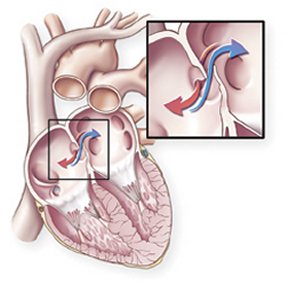

That opening functions in human fetuses to let the circulating blood bypass the lungs, which the body doesn’t rely on until a newborn starts breathing air. At or shortly after birth, tissue flaps in the heart usually fuse and close the hole. But in about a quarter of the U.S. population, complete closure never occurs.
The residual tunnel, called a patent foramen ovale (PFO), can act as a valve. It’s normally shut but occasionally shunts blood that’s headed to the lungs off to the brain and other parts of the body.
Most of the millions of people who have a PFO are never screened for it because doctors rarely suspect it of causing health problems. But in some cases, blood clots passing through the PFO can shoot to the head and trigger strokes. Air bubbles and dissolved chemicals can also slip through the one-way shunt rather than ride to the lungs, where they’d be exhaled or broken down.
To reduce the woman’s odds of another stroke, Sztajzel and his colleagues at the University Hospitals of Geneva performed surgery to close her PFO. According to the patient, her migraines immediately disappeared.
Sztajzel wasn’t the only researcher at that time to receive surprising new clues to a possible cause for migraines. Italian researchers had recently reported an unusually high prevalence of PFOs in people who suffer the headaches.
What’s more, at Royal Shrewsbury Hospital in England, cardiologist Peter Wilmshurst had found that scuba divers with PFOs were unusually susceptible to decompression sickness, a disorder that can occur when bubbles of nitrogen form in the blood and don’t get expelled by the lungs. After surgeons began fixing heart defects in some professional divers as a preventive measure against decompression sickness, several of them noted that their migraines disappeared. In 2000, Wilmshurst proposed that circulatory shunts, such as PFOs, can cause migraines, or at least those with aura.
Since then, Sztajzel and his colleagues, other Swiss researchers working independently, and teams of investigators in Italy, Belgium, and the United States have been examining that possibility.
Their findings are consistent in at least one respect: Sealing the heart defect often reduces the headaches. “There are now [at least] seven studies that show that closing your PFO cures your migraine or makes it better,” Wilmshurst says.
Recent innovations in medical technology have made closing a PFO safer and easier than it was even a few years ago. Cardiologists can now dam PFOs with devices that they thread up a vein to the heart from an incision in the groin. At some clinics, that operation doesn’t require general anesthesia or overnight hospitalization. Older techniques, by contrast, required surgically opening the rib cage.
Despite the promising findings and advances, most researchers don’t think that PFO closure is ready for prime-time use in treating migraines. They harbor lingering doubts because the studies thus far weren’t designed to rule out alternative explanations for the volunteers’ improvements.
Researchers also don’t know whether the findings apply to people with migraines but without strokes or other problems that have been previously associated with a PFO.
Several research teams have planned clinical trials that, within 2 years, could show whether PFO closure works against migraines. If these studies confirm the initial findings, millions of people in the United States could consider closure of the hole in their hearts as a treatment option for migraines.
Lights, action, headache
Migraines are throbbing headaches that, for many people, focus on one side of the head and often involve sensitivity to light, sound, and motion. Episodes can occur many times per month, and each can last a day or longer, says clinical research scientist Jill Jesurum of Swedish Medical Center in Seattle, who herself suffers migraines.
A minority of people with migraines experience sets of sensory signals, called auras, before each oncoming headache. A migraine’s aura can include imaginary lights, other vision disturbances, or numbness on one side of the body.
In any year, about 12 percent of the U.S. population experiences migraines. For reasons not fully understood but possibly related to female sex hormones, women make up three-quarters of that group. The headaches rarely occur before puberty but may begin—and can spontaneously end—at any point during adult life.
Triggers, which vary widely from one person to the next, include menstruation, stress, exertion, exposure to strong odors, lack of sleep, and missed meals. For many people, symptoms strike when several triggers converge, says Jesurum. For her, sleep deprivation and stress at work combine to set off migraine attacks.
Over recent decades, researchers have improved their understanding of the ways in which neurological activity and blood flow to the brain become disturbed during migraine attacks, says Vinod K. Gupta, a neurologist in Dubai, United Arab Emirates. But researchers have a limited grasp on the underlying biological processes that lead to those phenomena, he says.
Various classes of drugs—most of them originally designed to fight epilepsy, high blood pressure, or some other disorder—are used to treat people who have migraines. Yet neurologists’ expectations of success in quelling the headaches are generally modest, says cardiologist Mark Reisman of Seattle’s Swedish Medical Center.
Consider topiramate (Topamax), one drug now advertised as a migraine therapy. It reduces the frequency of attacks by an average of about 40 percent, but it can cause forgetfulness, fatigue, nausea, and skin sensations that have no apparent cause. That sort of trade-off is typical of many migraine drugs, Reisman says.
Heart and hole
In contrast to drugs, PFO closure appears highly effective against migraines and usually has no side effects, says Reisman, who has repaired the defect in more than 100 people. “We are seeing, in a number of patients, complete resolution of their headaches,” he says.
In the Feb. 15 Journal of the American College of Cardiology, Reisman, Jesurum, and their Seattle colleagues describe the results of 162 PFO closures in people with a history of stroke or related vascular blockages. Migraines had affected 57 of the patients before the operations. In more than half the patients who had been troubled with migraines, the headaches disappeared after the operation. Another 14 percent of patients reported a reduction by at least half in migraine frequency.
At a meeting of the American Heart Association in New Orleans last November, Sherman G. Sorensen of the Utah Heart Clinic in Salt Lake City and his colleagues reported on 121 stroke patients who’d had a PFO closed. Of the 69 people who’d had migraine headaches before the procedure, 30 had no headaches afterward and 27 reported partial relief from migraine symptoms.
As earlier studies had, these two tests relied on information that patients provided after PFO closure. So, it’s possible that the participants didn’t accurately remember the symptoms of their headaches. Or perhaps some aspect of the procedure, for example, the use of aspirin for several months after the operation, caused the improvement.
Nevertheless, researchers are excited by the possibility that PFOs cause some migraines. Wilmshurst speculates, “We think the PFO permits a substance that would be filtered in the lungs to get to the brain.” He and some other researchers suspect the peptide serotonin, which is neurologically active and doesn’t usually circulate in blood heading from the heart to the brain.
Some other possibilities are that small blood clots or debris temporarily but repeatedly blocks blood flow to a tiny portion of the brain. Such momentary events might not be evident as miniature strokes but could still set off abnormal neurological activity that leads to aura and other symptoms associated with migraines, says neurologist Stephen Landy, who runs the Wesley Headache Clinic and teaches at the University of Tennessee Medical School, both in Memphis.
Brain scans have shown evidence of such obstructions in some people with migraines, says neurologist Gian Paolo Anzola of Sant’Orsola Hospital in Brescia, Italy.
A study that he and his colleagues published in 2003 suggested that PFO closure is more effective against migraines with auras than against migraines without accompanying sensory signs.
Gupta remains skeptical that PFOs lead to migraines. He points out that some common medications for migraines lower blood concentrations of serotonin, but others raise it.
Landy, however, says, “It looks like there’s a definite relationship” between PFOs and migraines. But the mechanism “is still an enigma,” he says.
Good prospects
An estimated 28 million people in the United States get migraines, and studies of stroke survivors suggest that half of the people with migraines have PFOs. Therefore, devices used to close the heart opening represent “a tremendous market,” says cardiologist Bernhard Meier of University Hospital in Bern, Switzerland.
Two such devices are approved for use in the United States and a third is under review. At least eight are available in Europe. Any company that “has a working PFO device is looking into a bright future,” says Meier.
A trial, run by NMT Medical of Boston, that will compare the effects of PFO closure and other migraine treatments has begun in the United Kingdom. The initial study will focus on patients with aura for whom drugs don’t work well. That group represents about 5 percent of people with migraines.
The researchers plan to record volunteers’ migraine symptoms before and for at least 6 months after the operations.
NMT Medical intends to commence a parallel trial in the United States later this year. Other companies and university researchers are planning similar studies and may also test PFO closure in a more diverse group of people with migraines.
For some people, the results can’t come too soon. Meier and some of the other researchers say they’re already hearing from many patients with migraines who want to be tested for PFOs and, if possible, to have the operation.
“I would not recommend closure of PFO just for . . . migraine itself,” Gupta says. The data for migraines, unlike those for stroke, aren’t strong enough to prove a benefit of the heart procedure greater than the risks of the operation, he says.
Meier, however, says that he does PFO closures in patients with severe migraines who haven’t improved on medication. The risks must be considered carefully in each case, he notes. He says, “Migraine is not a deadly disease, [but] PFO closure could theoretically kill a patient.”
Anzola and his colleagues say that they close PFOs in people with migraines and no history of a stroke, but they perform the catheter procedure only in cases in which they find evidence of previously unrecognized, strokelike clots in the brain.
Among the researchers who have studied the effects of PFO closure on migraine, most—like Gupta—discourage people from seeking the treatment before more data become available. For now, these physicians close a PFO only when a patient has a history of stroke or another confirmed vascular problem. But many of the researchers are optimistic that future studies will endorse PFO closure for migraines.
If research bears out those expectations, what has been an uncommon procedure could become an important therapy in headache care.







