Will animal-to-human organ transplants overcome their complicated history?
A ‘breakthrough’ heart surgery earned acclaim, but it’s not clear how long the organ will work

In 2021, doctors at NYU Langone Transplant Institute transplanted a genetically modified pig kidney into a person who was clinically brain-dead to test how the human immune system would respond to the organ.
Joe Carrotta for NYU Langone Health
Editor’s note: After surviving for two months with a transplanted pig heart, David Bennett died March 8. “We have gained invaluable insights learning that the genetically modified pig heart can function well within the human body while the immune system is adequately suppressed,” transplant surgeon Muhammad Mohiuddin said in a statement released March 9 by the University of Maryland Medical Center, where the groundbreaking surgery was performed. “We remain optimistic and plan on continuing our work in future clinical trials.”
A 57-year-old Maryland man has now survived just over three weeks with the transplanted heart of a genetically engineered pig. His doctor has hailed the operation as a “breakthrough surgery” that could help solve the organ shortage crisis. But from a scientific standpoint, it’s too early in the game to know how much it moves the ball.
The use of animal organs for humans is an idea with a long, dramatic and often disappointing history (SN: 11/4/95). There’s an old saying about xenotransplantation, as the field is known, says Joe Leventhal, a surgeon who heads the kidney transplant program at Northwestern University Feinberg School of Medicine in Chicago. “It’s just around the corner. The problem is, it’s a very, very, very long corner.”
But a rash of new experiments, including three involving pig kidneys transplanted into people being kept temporarily alive on ventilators, has provided tantalizing evidence that achieving the decades-old ambition may finally be in reach.
The recent human operations come after an extensive effort to develop genetically altered pigs with organs that might avoid abrupt rejection, along with further refining of drugs that suppress the immune system and boost survival. That said, the Maryland heart operation was a Hail Mary rescue attempt and not part of a clinical trial — the kind of carefully designed study that is ultimately needed to show whether pig organs can function in humans, and do so safely.
One case can provide some valuable information about how the body responds to the organ, says Karen Maschke, a bioethics scholar at the Hastings Center in Garrison, N.Y., who is editor of Ethics & Human Research. “You may find stuff that you didn’t expect to find,” she says.
But a single snapshot of data doesn’t have enough context to draw conclusions, especially when it involves a gravely ill patient and brand-new technology. Without a study comparing several carefully selected patients, it’s hard to know whether one individual’s experience is typical.
Yet the latest flurry of pig-to-human transplant experiments could help open the door to the kinds of clinical trials that researchers want. That’s the only way to significantly advance the science, says heart surgeon David Cooper of Massachusetts General Hospital in Boston, who has long researched the idea of xenotransplantation. “We’ll learn much more if we are doing clinical cases than if we are staying in the laboratory.”
High on the hog
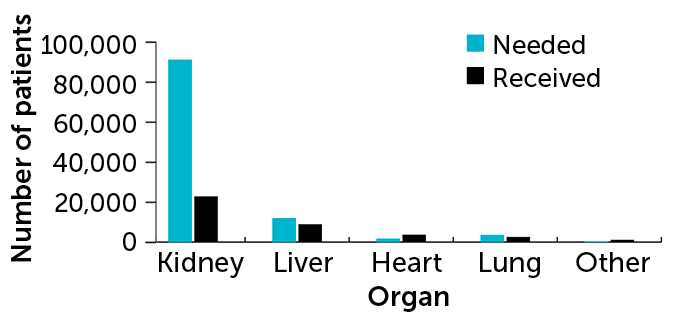
If clinical trials ultimately prove successful, animals could help ease a critical shortage of donor organs. Of the more than 106,000 Americans waiting for a transplant, around 90,000 need a kidney. Many will die before one is available.
Doctors have previously turned to animal organs in bold, headline-grabbing endeavors. Famed Houston heart surgeon Denton Cooley transplanted a sheep heart as a desperate move to save a dying man in the 1960s; the man’s body quickly rejected the organ.
One of the most high-profile tries at xenotransplantation occurred in 1984 when doctors at Loma Linda University Medical Center in California sewed a baboon heart into a 2-week-old baby born with a fatal cardiac defect (SN: 11/3/84). Baby Fae, as she was known, lived for 21 days and her surgery left a wake of controversy. Some medical ethicists called the operation a “beastly business” that lacked moral clarity. Scientists “beat a hasty retreat back to the laboratory,” according to a 1995 report in the Journal of the American Medical Association.

More recently, scientists have focused on pigs, largely because porcine organs are about the size of adult humans’, and the animals are already raised on an industrial scale. Still, the feasibility of the idea was thrown into doubt with the discovery in the 1980s that pig cells are coated with a type of sugar molecule, called alpha-gal, that strongly triggers the human immune system.
The field also experienced a setback with the discovery in the 1990s that the swine genome contains embedded viruses, snippets of viral genetic code woven into pigs’ genetic instruction books. (It’s not just a pig trait; these kinds of viral genes make up an estimated 8 percent of the human genome too.) The viruses, called porcine endogenous retroviruses, don’t bother pigs but might cause problems after suddenly finding themselves in another species.
In the early 2000s, researchers reported the creation of genetically modified pigs lacking alpha-gal, making them theoretically more compatible with the human immune system than a hog straight from the farm. That announcement set off attempts to raise alpha-gal-free animals, most notably in the United States by Revivicor, a company owned by United Therapeutics, based in Blacksburg, Va. Then, in 2020, the possibility of pig-to-human transplants took a giant leap forward, when, for the first time, the U.S. Food and Drug Administration approved Revivicor pigs for human use.
Xenotransplantation also got a boon from CRISPR/Cas9 gene-editing technology and its remarkable ability to snip genes at will. Using CRISPR, scientists can trim the unwanted viral genes from pigs (SN: 8/10/17). “Gene editing with CRISPR has just really helped accelerate the field in sort of a warp drive,” Leventhal says.
In recent experiments, pig kidneys and hearts have been successfully transplanted into baboons. Though the baboons died within days in early xenotransplantation attempts, researchers reported in 2018 that transplanted pig hearts kept beating in the chests of two baboons for about six months, a record at the time (SN: 12/5/18). Other similar experiments have replicated that survival time.
Then, in October 2021, scientists from NYU Langone Health in New York City made the jump to humans: In a test, they grafted a Revivicor kidney onto a person who was clinically brain-dead and watched the organ function for 54 hours, presumably long enough to detect any signs of immediate rejection (SN: 10/22/21). Less than two months later, the same surgical team repeated the experiment. A third such transplant from researchers at the University of Alabama at Birmingham, this time into the abdomen of a man kept temporarily alive by a ventilator following a motorcycle accident, was described January 20 in the American Journal of Transplantation.
None of the kidneys transplanted in people appeared to provoke immediate immune rejection, and the organs even began to produce urine, doctors reported. Given the overwhelming need for kidneys, and proof-of-concept renal tests already done, most experts predicted that the first modern patient to get a xenotransplant would need a kidney.
Then came the unexpected news of David Bennett.
‘I want to live’
Bennett was suffering from acute heart failure and did not qualify for the human heart transplant list. On New Year’s Eve, the FDA gave doctors from the University of Maryland Medical Center permission to transplant the pig heart through a special protocol, sometimes called compassionate use, that allows very sick people emergency access to experimental drugs or devices — either because the patient doesn’t qualify for any study of the drugs or because no study exists. Bennett’s new heart also came from a Revivicor pig.
In a statement issued by the hospital, Bennett said he consented to the experimental surgery because he was simply out of options. He was bedridden, and no hospital would offer him a heart transplant, at least in part because he had a history of not following medical advice. “It was either die or do this transplant,” he said. “I want to live.” The eight-hour operation was performed on January 7.

A little over three weeks later, Bennett is gaining strength, says Muhammad Mohiuddin, a surgeon who directs the cardiac xenotransplantation program at the hospital and who was part of the surgical team. Everyday accomplishments, like talking with the staff about football playoffs, are tiny victories.
“We are counting all these smaller wins and hope this heart will keep supporting him,” Mohiuddin says. The heart is strong enough that the doctors have had to dampen its power because it was too much for Bennett’s body, weakened from lying in bed for weeks. “We put a Ferrari engine in a 1960 car,” Mohiuddin says.
Still, Cooper, from Massachusetts General, said he was surprised when he learned that the first living pig-to-human transplant patient received a heart, not a kidney. “What are they going to do if this graft slowly begins to fail?” he asks. “There’s going to be a little bit of a problem.”
“I thought it would be the kidney first. Because if that fails — say you get rejection that you didn’t expect, or you get infection that you can’t manage — you can take the kidney out, stop all the immunosuppressive therapy and put the patient back on dialysis.” A heart transplant is not so reversible.
Cooper and surgeon Hidetaka Hara, who were at the University of Alabama at Birmingham together, had suggested that the first xenotransplant should be a step-by-step clinical trial with four patients waiting for a kidney. The trial would work like this: Three months after the first patient receives a transplant, perform the operation in a second patient if the first person isn’t having complications. If those two are doing well, transplant a third pig kidney three months later, and a fourth three months after that, the pair laid out in September in EBioMedicine. “So over the course of a year,” Cooper says, “you’ve followed up four patients and you can see whether are they all doing well or are there complications.”
Starting a clinical trial with kidneys also makes sense, Cooper says, because the need is so much greater. Around 83 percent of the transplant waiting list are people who need kidneys; 3 percent need a heart.
That’s why eGenesis, a company in Cambridge, Mass., is focusing its research efforts on kidneys. “It’s where the dominant need is,” says Mike Curtis, the company’s president of research and development. eGenesis, which is raising gene-edited, immune-compatible pigs, hopes to begin a clinical trial of six to 10 patients with transplanted pig kidneys around 2024.
Mohiuddin says that the reason he performed a heart operation is simple: He’s a cardiac surgeon, and the patient was dying. “My 30-year interest has been only in hearts,” he says. His research team has approached the FDA for permission to do a clinical trial, he says, but the agency wants more consistent data from baboon studies first. “We hope to get that permission,” he says. “This was just to save Mr. Bennett’s life.”
One and not done
Should Bennett check out of the hospital and go home, that high-profile milestone could serve a purpose beyond allowing him more time with his family: It could help persuade the FDA to green-light a larger, scientifically designed trial, Cooper says.
If Bennett continues doing well, doctors “may be able to get a handful of [heart] patients done over the next few months. And then they go back to the FDA and say, look, these patients generally did well. Now can we do a proper series, where we take patients on our own waiting list and do the transplants?”
Leventhal, the surgeon from Northwestern, has the same hope about approved clinical trials. “The only way that you’re going to see whether these organs provide meaningful function over the long term in humans, in a way that would justify their use, is to transplant them into humans and follow them longer-term.”
Still, it remains to be seen whether that will occur under compassionate use, as Bennett received, or in formal studies. The FDA’s expanded access provision was designed to help people obtain drugs and procedures that they couldn’t normally get. “Whether it should have been used in the case of an organ is an interesting ethical and regulatory and policy question,” Maschke, the bioethicist, says.
“One of the problems with going the route they did is that there are probably hundreds of heart patients in the country who are not on a waiting list because they’re too sick,” Maschke says. “Some of those folks may say, ‘I’ll never take an animal organ,’ but some of them might say, ‘Yes, I would take a pig heart. I want to do this too. Can you get me access?’”
Waiting game
In the United States, the large majority of people on the transplant waiting list need kidneys. Kidney transplants are also the most common type of transplant performed.
Number of people on a waiting list vs. transplants performed, by organ in 2020
But opening the floodgates could make it harder to find volunteers for clinical studies. And in some cases, it could backfire. That’s what happened in the 1990s when doctors started offering women with advanced breast cancer massive doses of chemotherapy followed by bone marrow transplantation to restore their collapsed immune systems. Thousands of women received the experimental treatment — so many that scientists had trouble recruiting for studies. And when the scientific trials were finally done, the treatment showed no benefit.
That’s why there’s often a concern about moving too fast, “because you don’t want to derail the science — and the science is incremental,” Maschke says.
For now, pig-to-human transplantation has logistical issues that will help restrict its use. For one, the painstakingly engineered pigs are hard to come by. In addition to their rare genetic pedigree, they must be raised in sterile environments so they don’t pick up any microbes that might be transferred to humans. Another possible hurdle: Animal rights groups have decried the idea of pigs as spare parts for humans as “cruel and dangerous,” a sentiment that society will need to square with the urgent medical need.
But first, doctors need to know if xenotransplantation is even possible, or will once again end in failure. “What we don’t know is, how long and how well will these organs work in patients?” Leventhal says. “The only way we’re going to assess that is through transplanting them.”







