Boosting a gut bacterium helps mice fight an ALS-like disease
People with Lou Gherig's disease appear to have a dearth of the microbes
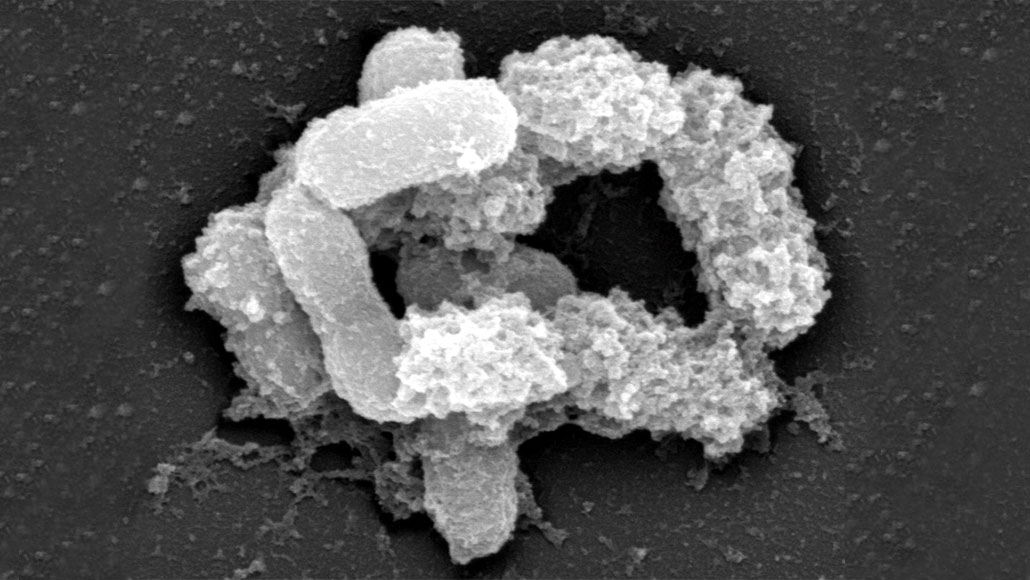
BACTERIAL BUDDY Gut bacteria called Akkermansia (shown in an electron micrograph) produce vitamins and other molecules that lessen the severity of ALS symptoms in mice. People with ALS have fewer of these bacteria than healthy people do, but it’s too soon to tell whether getting more of the bacteria or its products will help.
Patrice Cani/UCLouvain







