Fentanyl’s death toll is rising
Opioid’s ability to freeze chest muscles within minutes may be to blame for some overdoses
FATAL ATTRACTION The ability of fentanyl, an opioid, to freeze chest muscles within minutes may be to blame for some overdoses, a new autopsy study shows.
© Julia Hiebaum/Alamy Stock Photo
For some people, fentanyl can be a life-saver, easing profound pain. But outside of a doctor’s office, the powerful opioid drug is also a covert killer.
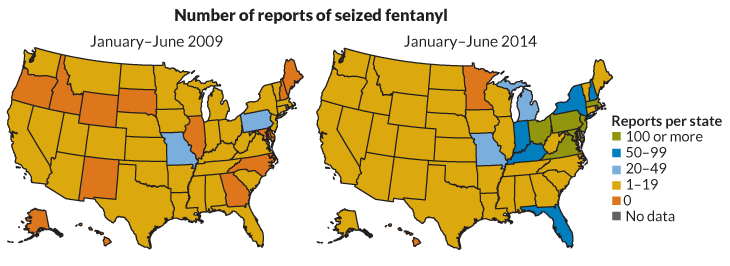
In the last several years, clandestine drugmakers have begun experimenting with this ingredient, baking it into drugs sold on the streets, most notably heroin. Fentanyl and closely related compounds have “literally invaded the entire heroin supply,” says medical toxicologist Lewis Nelson of New York University Langone Medical Center.
Fentanyl is showing up in other drugs, too. In San Francisco’s Bay Area in March, high doses of fentanyl were laced into counterfeit versions of the pain pill Norco. In January, fentanyl was found in illegal pills sold as oxycodone in New Jersey. And in late 2015, fentanyl turned up in fake Xanax pills in California.
This ubiquitous recipe-tinkering makes it impossible for users to know whether they’re about to take drugs mixed with fentanyl. And that uncertainty has proved deadly. Fentanyl-related deaths are rising sharply in multiple areas. National numbers are hard to come by, but in many regions around the United States, fentanyl-related fatalities have soared in recent years.
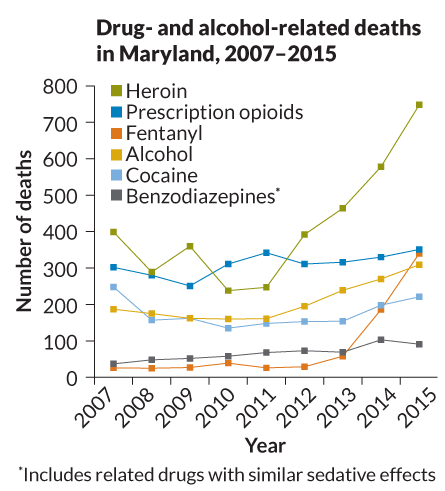
Maryland is one of the hardest-hit states. From 2007 to 2012, the number of fentanyl-related deaths hovered around 30 per year. By 2015, that number had grown to 340. A similar rise is obvious in Connecticut, where in 2012, there were 14 fentanyl-related deaths. In 2015, that number was 188.
In Massachusetts, two-thirds of people who died from opioid overdoses in the first half of 2016 showed signs of fentanyl. This wave of fentanyl-related overdoses is “horrendous,” says Daniel Ciccarone of the University of California, San Francisco. What’s worse, he says, “I think it’s here to stay.”
Fentanyl is not a new drug. Available in the 1960s, it is still used in hospitals as an anesthetic and is available by prescription to fight powerful pain. What’s new, Ciccarone says, is that clandestine drug manufacturers have discovered that the euphoria-producing opioid can be made cheaply and easily — no poppy fields necessary.
Fentanyl is about 30 to 40 times stronger than heroin and up to 100 times more powerful than morphine, which means that a given effect on the body can be achieved with a much smaller amount of fentanyl. Inadvertently taking a bit of fentanyl can cause big trouble. “It’s a dosing problem,” Nelson says. “Because the drug is so potent, little changes in measurements can have very big implications for toxicity. That’s really the problem.”
That problem is made worse by the variability of illegal drugs — users often don’t know what they’re buying. Illegal labs aren’t pumping out products with carefully calibrated doses or uniform chemical makeup. The drugs change from day to day, making it nearly impossible for a user to know what he or she is about to take, Ciccarone says.
He has seen this struggle up close. Drug users have told him that the products they buy are unpredictable. Another thing people are telling him: “That they and their friends and compatriots are dropping like flies.” Tellingly, some of the most experienced drug users have recently begun doing “tester shots,” small doses to get a sense of the type and dose of drug they’re about to use, Ciccarone says.
Users are right to be wary. Typically, opioids can kill by gradually depressing a person’s ability to breathe. Illicit fentanyl, a recent study suggests, can kill within minutes by paralyzing muscles. Doctors have known that when injected quickly, fentanyl can paralyze chest wall muscles, prevent breathing and kill a person rapidly. That effect, called “wooden chest,” might help explain the rise in fentanyl-related deaths, scientists report in the June Clinical Toxicology.
A quick injection of fentanyl “literally freezes the muscles and you can’t move the chest,” says toxicologist Henry Spiller of the Central Ohio Poison Center in Columbus. That’s why doctors who dispense fentanyl in the hospital intentionally proceed very slowly and keep the opioid-counteracting drug naloxone (Narcan) on hand. “If you give it too fast, we know this occurs,” Spiller says. But it wasn’t known whether this same phenomenon might help explain the death rate of people using the drug illegally.
Spiller and colleagues tested post-mortem concentrations of fentanyl and its breakdown product norfentanyl in 48 fentanyl-related deaths. The body usually begins breaking down fentanyl into norfentanyl within two minutes, an earlier study found. Yet in 20 of the cases, the researchers found no signs of norfentanyl, indicating death came almost immediately after first receiving fentanyl.
Naloxone can counteract the effects of opioids if someone nearby can administer the antidote. But for people whose chests quickly freeze from fentanyl, resuscitation becomes more unlikely. Fentanyl “is just a bad drug,” Spiller says.
Story continues below maps
Fentanyl’s danger is magnified for people not accustomed to taking opioids, such as those addicted to cocaine, a situation illustrated by a recent tragedy in New Haven, Conn.
New Haven authorities noticed a string of suspicious overdoses in late June, leaving three people dead. Drug users thought they were buying cocaine, but the drugs contained fentanyl, says analytical toxicologist Kara Lynch of the University of California, San Francisco. As one of the handful of labs capable of testing blood and urine for fentanyl, hers was called on to identify the culprit. Her lab spotted fentanyl in Norco tablets back in March.
Lynch’s group uses high-resolution mass spectrometry to detect many drugs’ chemical signatures. But this method reveals only the drugs scientists suspect. “We can look for what we know to look for,” she says. And success depends on getting the samples in the first place.
The logistical hurdles of figuring out exactly what a person took, and how much, and when, are large. Ciccarone contrasts the situation with cases of food poisoning. When people start getting sick, public health officials can figure out what lettuce people ate and test it for pathogens. The same kind of tracking system doesn’t exist for drugs. His efforts to develop a system for testing illegal drugs in Baltimore broke down in part because no one had time to do the work. “The coroner is so busy right now with dead bodies,” he says. “They don’t have the time to test the ‘lettuce.’ ”
In the quest to curb fentanyl-related deaths, scientists and public health officials are searching for new strategies. Spiller advocates a more targeted public health message to users, one that emphasizes that fentanyl is simply a deadly drug, not just a more potent high. Ciccarone says that facilities where drug users can take illegal drugs under the care of medical personnel might reduce the number of fatalities.
For now, the scope of the problem continues to grow, Nelson says. The situation is made worse by the ingenuity of illicit drugmakers, who readily experiment with new compounds. Fentanyl itself can be tweaked to create at least 16 related forms, one of which, acetyl fentanyl, has been linked to overdose deaths. New drugs and new tweaks to old drugs rapidly evolve (SN: 5/16/15, p. 22), Nelson says, creating a game of whack-a-mole in which designer drugs confound public health officials and law enforcement.
“There is no single easy solution to this problem,” he says.