Harmless bacterium edges out intestinal germ
Clostridium scindens inhibits closely related microbe C. difficile
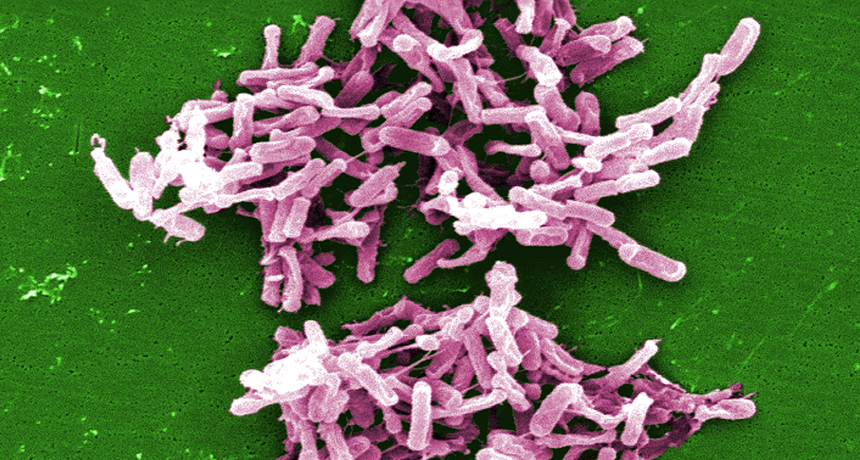
BACTERIA VS. BACTERIA Mice exposed to Clostridium difficile (shown) are protected by a related microbe, C. scindens.
Janice Haney Carr/CDC
- More than 2 years ago
Gut infections from the bacterium Clostridium difficile can be fought with a closely related but harmless microbe known as C. scindens. The friendly bacterium combats infection in mice by converting molecules produced in the liver into forms that inhibit C. difficile growth, researchers report October 22 in Nature.
C. scindens also appears to protect people from infection, the researchers found in a preliminary study in humans.
The new findings could begin a path to the next generation of therapies using gut bacteria, says Alexander Khoruts, a gastroenterologist at the University of Minnesota in Minneapolis.
People who become infected with C. difficile typically have taken antibiotics, which wipe out the beneficial microbes in the gut, giving C. difficile a chance to take root. The infection can lead to cramps, diarrhea and even death. An estimated 500,000 to 1 million people get C. difficile infections each year in the United States. People with C. difficile receive more antibiotics to treat the infection or a fecal transplant to restore healthy microbes to the gut.
Several research groups have been trying to identify gut bacteria that are resilient in the face of C. difficile so that physicians can give patients those bacteria as a treatment, says Eric Pamer, an immunologist at Memorial Sloan Kettering Cancer Center. Single strains of bacteria such as C. scindens would offer significant advantages over fecal transplants: With a transplant, doctors screen the donated feces for pathogens that might sicken the recipient. But, Pamer says, “there are many things, viruses that have yet to be identified, that could be in a crude fecal product that might cause trouble.”
Pamer and his team gave mice antibiotics to deplete beneficial microbes but not wipe them out completely. The researchers then fed the mice C. difficile spores and identified microbes that appeared in mice with lower amounts of C. difficile in their guts. C. scindens was the clear victor. It is harmless and present in most people, but in very low numbers.
The researchers then grew C. scindens and fed the bacteria to mice before exposing them to C. difficile. Compared with mice that received no microbes, the C. scindens-fed mice ended up with lower amounts of C. difficile in their guts, lost less weight and were less likely to die.
The researchers also examined the microbial populations of 24 patients undergoing stem cell transplants. Those patients had lowered microbial diversity after receiving combinations of antibiotics, radiation and chemotherapy. The patients who didn’t develop C. difficile after the transplant were more likely to have C. scindens in their guts.
“This is a pretty big leap forward in figuring out why people are resistant or sensitive to infection,” says Joseph Sorg, a microbiologist at Texas A&M University in College Station.
The researchers also investigated how C. scindens combats C. difficile.
C. difficile begins growing after it is exposed to certain molecules secreted in bile after a meal. However, another form of the molecule inhibits C. difficile growth. C. scindens transforms the molecule from one form to the other, boosting resistance to C. difficile.
Eventually, the researchers plan to see if C. scindens combats C. difficile in human studies. The bacteria could bolster patients’ resistance to C. difficile before the infection takes hold.







