Life in Print
Cell by cell, ink-jet printing builds living tissues
Almost as soon as ink-jet printers hit the market in the 1980s, materials researchers realized that the machines could be used to deposit droplets of substances other than ink. In principle, anything that could squeeze through the printhead—including plastics, silicon, or dissolved metals—could be laid out in some precise pattern. And when printed in layers to create three-dimensional structures, such “inks” could allow the rapid design and even production of plastic or electronic parts for a variety of devices (SN: 3/27/04, p. 196).
If ink-jet technology could work for printing plastic and electronic components, researchers suggested, it could also work for custom designing structures built with living cells.
“One of our goals, in a sense, always was to build a mechanical rat—if we can have moving parts, structural parts, and electrical parts all in one unit, then it’s kind of like an animal,” says Paul Calvert of the University of Massachusetts Dartmouth. “If I can build a mechanical rat, then maybe I could build a real rat.”
Ink-jet printers won’t start out by mass-producing living rats, though. Instead, researchers are setting their sights on producing skin, heart-muscle patches, and perhaps even organs.
Although researchers can create intricate structures with ink-jet printing, organs built in this way might not perform perfectly, because engineered tissues do not go through a natural development process, says Thomas Boland of Clemson University in South Carolina. Natural tissues follow a bottom-up design, developing through the growth and differentiation of various progenitor cells. Engineered tissues instead conform to a top-down design template, based on what a final tissue should look like. Though the designs provide an overall structure, researchers rely on the cells’ biology to fill in that template and signal to each other to produce an organized tissue.
Even though ink-jet–printed tissues might not have the same properties as their natural counterparts, such structures could prove useful in medicine and even in novel devices. Ink-jet tissues could provide new cell-based materials for drug testing, new ways to probe cellular communication, living sensors, or even fuel cell–type batteries.
Printing cells
Most inexpensive home printers signal a tiny nozzle to heat the ink just enough to build up pressure so that it releases a droplet that falls onto the page. More expensive industrial printers deposit an ink droplet when a piezoelectric crystal within the nozzle vibrates in response to an electric current. Because of the sensitivity of cells to heat, electricity, and other stresses, it might seem that cells couldn’t survive such arduous treatment.
In fact, experiments show that at least 90 percent of cells can survive the printing process and remain viable. Boland and his colleagues have used modified thermal ink-jet printers to print mammalian cells, including human neurons and cardiac cells, onto biopaper, a hydrated gel surface made of collagen. Other groups, including Brian Derby’s at the University of Manchester in the United Kingdom, use piezoelectric printers. Derby and his colleague, cell biologist Julie Gough, recently demonstrated survival rates of 95 percent or better when they printed human fibroblasts.
Such systems allow researchers to place cells individually and precisely. For example, Derby’s ink drops are 10 to 50 micrometers (µm) across and have a volume of roughly 10 picoliters, or one 100-billionth of a liter. With cells measuring approximately 8 to 10µm across, each drop probably contains one cell on average, he says. Simple modifications can tweak a conventional office printer to print those individual cells in layers, one on top of another, to produce 3-D structures, Boland says.
Arranging cells in three dimensions is only the first step, however. Such structures need materials around the cells that will support and sustain them, and a major challenge is producing inks with the appropriate properties for building robust 3-D structures. These inks, separate from the ones that deposit cells, have to be liquid within the printer but then solidify once they’re released in drops from the printer. They also need to mimic the natural rigidity and flexibility of tissues. Researchers are investigating materials that are compatible with the cells and that switch their properties depending on temperature or some other controllable factor. To boost cell survival in the scaffolds, they may need additional proteins such as growth factors and agents that prompt cells to specialize. “We still have a long way to go to optimize the ink for these materials,” Boland says. Several groups are teaming with printer manufacturers to develop printers tailored to cell-based applications.
Cellular communication
Although cells suspended in a medium can move through a printer just like any other ink, introducing a living ingredient produces a dynamic material. The cells respond to each other as well as to chemicals included in the printing mixture to influence cell behavior. Chemical signals between cells are critical for organizing and maintaining complex tissues, but researchers know relatively little about how extracellular signals work together. Scientists understand how certain signals lead cells to grow, divide, and produce the complex patterns within living tissues, Calvert says, but they don’t know “how this allows different cell types to wind up in the right structure.”
Continuing studies with cell printing will help researchers understand the chemical signals that enable different cells to work together to build a functioning tissue. “We’re building sandwiches, putting down a layer of cells, then a separator, and another layer of cells,” Calvert says. By examining how the second layer of cells responds to the first and by analyzing the molecular signals between them, biologists may be able to track how cells move and change in response to other cells, and isolate the signals responsible for particular cellular behaviors.
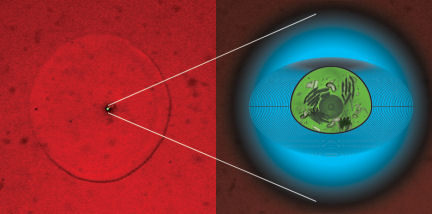
Ink-jet printers can also build test systems to study chemicals involved in stem cell differentiation. Researchers at Carnegie Mellon University in Pittsburgh and at the University of Pittsburgh printed gridlike patterns of an ink containing a bone-differentiation factor. When they later added muscle-derived stem cells to the surface, bone cells developed only in the squares with the bone-differentiating factor. Cells in other areas developed into musclelike tissue. “We’re trying to understand the basic biology,” says Julie Phillippi of the University of Pittsburgh, “before we can translate it into a therapy.”
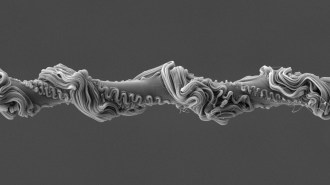
Cells can do more than simply respond to chemicals in their environment; sometimes they can help their scaffolding structures organize around them. In their effort to build sensing devices, C. Jeffrey Brinker and his colleagues at Sandia National Laboratories and the University of New Mexico in Albuquerque have used methods that include ink-jet printing to build silica-based structures incorporating molecules such as lipids that contain both water-attracting and water-repelling portions. Such molecules create a defined nanoscale structure within the glassy material. When the printer deposited yeast or bacterial cells onto these silica-lipid structures, “the cell kind of co-opted the system,” Brinker says. “It intervened in the self-assembly process and created a rather unique interface between itself and the silica matrix.” Each cell organized the lipid molecules in its immediate vicinity so as to create and maintain a less acidic environment within a few micrometers of the cell wall.
“The feature that we like about our process is that the [silica-lipid] matrix develops in a 3-D sense around the cell,” Brinker says. Altering the components within their glassy material gives the cells within the system tools to organize different structures with potentially new characteristics. Although Brinker still doesn’t completely understand how the cell reorganizes the matrix components, he and his colleagues are extending their experiments to include more-delicate mammalian cells within their synthetic scaffold.
Synthetic structures seeded with cells could serve as the foundation of “living” devices such as cell-driven batteries or sensors to test how particular cell types react when they encounter a toxic substance. Ink-jet–printed tissues are likely to serve a similar role as test materials for drugs or other substances long before they make it to the clinic as replacement tissues, say Boland and Calvert.
Building vessels
As researchers strive to print thicker and more-complex tissues with an ink-jet, they will have to solve a fundamental plumbing problem. Unlike layers of plastic, silicon, or metal assembled to form a synthetic device, cells located away from a tissue surface cannot survive without nutrients. In natural tissues, cells are no more than 100µm from a capillary that supplies oxygen and nutrients, says Derby. Diffusion allows those chemicals to travel up to a millimeter at most. “We’re limited in thickness until we can build a plumbing system in there,” Derby says. Building structures that mimic natural blood vessels will involve printing a variety of cell types in cylindrical forms, with both the sturdiness and flexibility to deliver blood or other liquid nutrients.
Building vessel-like structures has been tougher than anticipated, Boland says. One option for building an isolated blood vessel is to print a two-dimensional sheet of cells and then roll it into a tube. But printing blood vessels within complex tissue is a resolution problem, comparable to that of printing a high-resolution photograph, in which very small ink dots in four colors sit adjacent to each other to produce a crisp image with millions of colors. Print the dots too close together, and they will smudge and create a blurred picture. Similarly, creating complex structures with cells requires printing different cell types close together but also in such a way that they form discrete functional structures.
To construct integrated blood vessels, Boland and his colleagues first built a foundation layer containing protein. Then they print a mixture of cross-linking chemicals and blood vessel–forming cells that form pores as the drops strike and cause the surface to set. If researchers print these drops fast enough and close enough together, the pores can coalesce to form channels and trap the cells inside, Boland says. Those trapped cells then divide and form vessels within the channel structures. This ability to place cells precisely and to separate different cell types will be important for building and studying 3-D cell culture and even for building organs, he adds.
But researchers don’t have all the plumbing built yet to connect these vessels to larger ones. “We’ve done some functional studies, but the [printed] vessels are so small that it’s impossible to connect them into a blood vessel,” Boland says. The engineered blood vessels are 30µm or less across—so small that a surgeon couldn’t link them to living vessels in a patient. “We’re confident that we’ll get there,” Boland says. “At that point we’ll hook it up to either to an animal or in vitro to media or blood through a pump.”
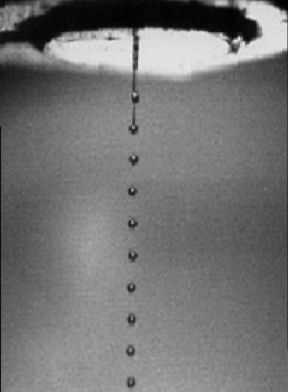
Because of the complexity of building multicellular structures and blood vessels, some researchers are aiming to assemble tissue structures by starting with larger, prefabricated chunks of tissues called bio-ink particles. The larger pieces of tissue don’t require the scaffolding materials needed for traditional tissue engineering or for ink-jet strategies that print single cells, says Gabor Forgacs of the University of Missouri at Columbia.
Forgacs and his colleagues are using this strategy to build blood vessels that contain three basic types of cells: endothelial cells, which line the vessel; smooth muscle cells, which give elasticity; and fibroblasts, which produce chemicals outside the cell that give vessels their sturdiness. First, researchers culture the different cell types and then combine them to make the individual bio-ink particles, up to 500µm across.
The researchers use a micropipette system similar to an ink-jet to place the bio-ink particles like blocks to build up sheetlike or cylindrical structures similar to blood vessels.
Pumping cell-culture media through the cylindrical structure as blood would flow through a vessel cues the cells to move to their appropriate locations. Endothelial cells migrate to the inner surface of the vessel, muscle cells to the middle, and fibroblasts to the outer layer. “We control the deposition of bio-ink particles. We control the composition of bio-ink particles, but that’s basically it,” Forgacs says. “After that, nature takes over and completes the job.”
Though the principles look promising for building blood vessel–like structures and other tubular tissues such as the gut, the scientists are still testing how such tissues would perform under physical stresses comparable to those within a living organism. Using bio-ink particles composed of heart cells from chickens and endothelial cells from human blood vessels, Forgacs and his colleagues have created tissuelike structures that beat, they report in an upcoming Tissue Engineering. The tissues included structures that resembled blood vessels in an early stage of development.
Tissue replacements
Though confident that they will eventually figure out how to circulate nutrients within thicker tissues, researchers say that complex replacement organs such as hearts or lungs are decades away. Printed tissues might enter the clinic in the nearer future as patches of heart muscle, for example, that involve a limited number of cell types, Boland says.
Still, researchers are optimistic that ink-jet printing will produce products that will eventually help patients whose organs have failed. “We might be able to print all kinds of organs or invent new organs. They might do a job, but they probably will never replace the original,” Boland says. “But they could make a real difference in quality of life” for some patients.
Sarah Webb is a freelance writer in New York.