Long COVID brain fog may be due to damaged blood vessels in the brain
The result suggests there is a biological basis for this symptom

Brain fog is a debilitating symptom commonly reported by people with long COVID. Now, scientists have linked the symptom to leaky boundaries in the brain.
baona/iStock/Getty Images PlusLeakiness in the brain could explain the memory and concentration problems linked to long COVID.
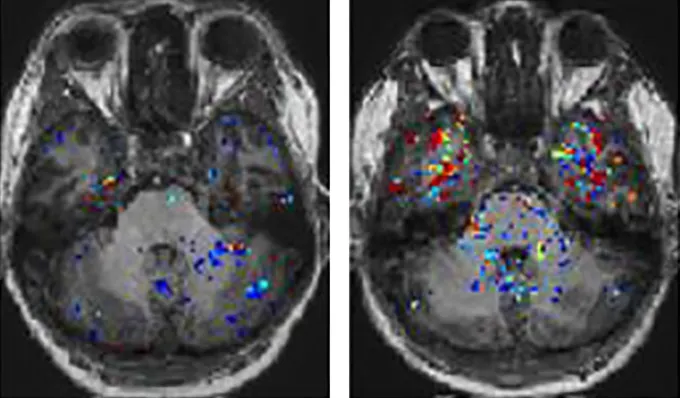
In patients with brain fog, MRI scans revealed signs of damaged blood vessels in their brains, researchers reported February 22 in Nature Neuroscience. In these people, dye injected into the bloodstream leaked into their brains and pooled in regions that play roles in language, memory, mood and vision.
It’s the first time anyone’s shown that long COVID patients can have leaky blood brain barriers, says study coauthor Matthew Campbell, a geneticist at Trinity College Dublin in Ireland. That barrier, tightly knit cells lining blood vessels, typically keeps riffraff out of the brain, like bouncers guarding a nightclub.
If the barrier breaks down, bloodborne viruses, cells and other interlopers can sneak into the brain’s tissues and wreak havoc, says Avindra Nath, a neurologist at the National Institutes of Health in Bethesda, Md. It’s too early to say definitively whether that’s happening in people with long COVID, but the new study provides evidence that “brain fog has a biological basis,” says Nath, who wasn’t involved with the work. That alone is important for patients, he says, because their symptoms may be otherwise discounted by physicians.
For some people, brain fog can feel like a slowdown in thinking or difficulty recalling short-term memories, Campbell says. For example, “patients will go for a drive, and forget where they’re driving to.” That might sound trivial, he says, but it actually pushes people into panic mode.
Campbell’s team studies repetitive head trauma. They knew that traumatic brain injuries can disrupt the blood brain barrier — and that people with these injuries sometimes report having brain fog. That mental muddling reminded the team of what people with long COVID can experience. Maybe the blood brain barrier disruption seen in some concussion patients applies to long COVID brain fog, too, the researchers surmised.
Evidence for SARS-CoV-2’s damaging effects on the brain has been mounting for years. Studies in cells and animals suggest the virus can crumble components of the blood brain barrier. And autopsies of people who have died from COVID-19 reveal barrier breakdowns, Nath and others have shown.
But until now, no one knew if this kind of damage persisted long after the initial infection subsided. The team scanned the brains of 32 people, 10 of whom had recovered from COVID-19, and 22 with long COVID. Of those with long COVID, half reported having brain fog.
An injected dye lit up all the participants’ brains during MRI brain scans. In people recovered from COVID, the dye had trouble crossing the blood brain barrier. Likewise, in long COVID patients without brain fog, the dye mostly stayed put, confined within blood vessels. But in eight of 11 participants with brain fog, the dye tended to escape from blood vessels and enter brain tissue.
“It was just so clear,” Campbell says. He remembers one of the first people scanned, someone with severe brain fog. Their temporal lobes, brain regions that sit behind the eyes, were “just flooded with this dye,” he says. The researchers’ work suggests that “brain fog wasn’t just a figment of [patients’] imagination,” Campbell says. “It was a very, very real thing that they were reporting.”
The new findings offer an opportunity to think about potential therapies, Nath says. Perhaps researchers can find a way to slow down the blood brain barrier’s breakdown — or reverse it.







