Monkeypox is not a global health emergency for now, WHO says
Meanwhile, scientists are analyzing the virus’s genetic data for clues to its unprecedented spread
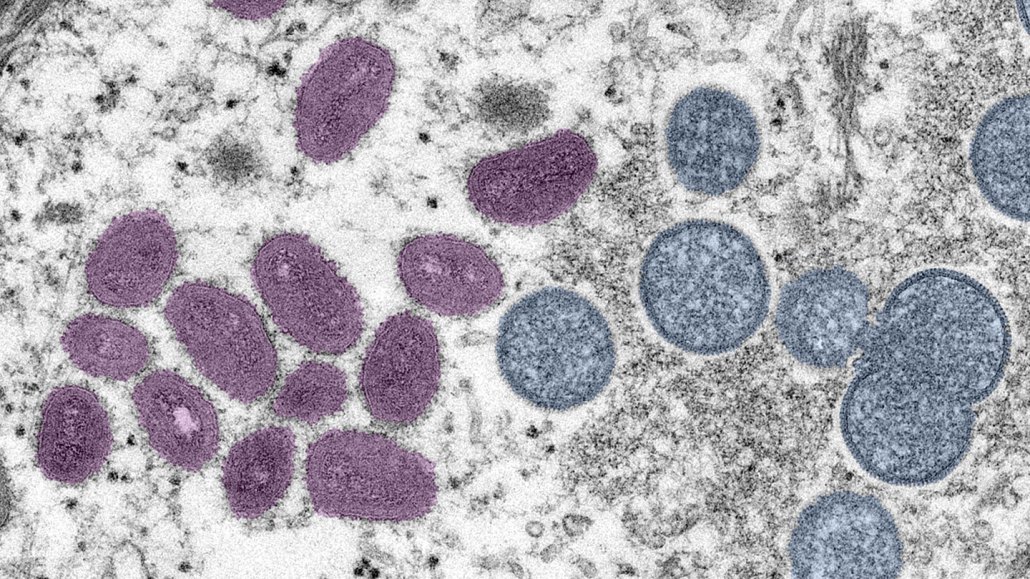
Monkeypox has spread to at least 4,100 people in 46 countries. Mature monkeypox viruses, pink, and immature viruses, blue, are shown in a colorized electron micrograph.
Cynthia S. Goldsmith, Russell Regnery and Hannah Bullock/CDC
Monkeypox is not yet a global public health emergency, the World Health Organization said June 25.
The decision comes as the outbreak of the disease related to smallpox continues to spread, affecting at least 4,100 people in 46 countries as of June 24. That includes at least 201 cases in the United States. Those cases have been found in 25 states and the District of Columbia, according to the U.S. Centers for Disease Control and Prevention.
“Controlling the further spread of outbreak requires intense response efforts,” and the situation should be reevaluated in a few weeks, the WHO committee evaluating the outbreak said in an announcement.
The declaration of a public health emergency would have potentially made it easier to get treatments and vaccines to people infected with or exposed to the virus. Some medications and vaccines that could help fend off monkeypox are approved for use against smallpox, and can be used against monkeypox only with special authorization.
The virus that causes monkeypox, named for its discovery in monkeys in 1958 though it is probably a virus that mainly infects rodents, is not a new threat. Countries in central Africa, where monkeypox is endemic, have had sporadic outbreaks since researchers found the first human case in 1970. Places in western Africa had few cases until 2017. But most cases outside the continent were travel-related, with limited spread to others (SN: 5/26/22).
“Monkeypox has been circulating in a number of African countries for decades and has been neglected in terms of research, attention and funding,” WHO director-general Tedros Ghebreyesus said in a statement announcing the decision. “This must change not just for monkeypox but for other neglected diseases in low-income countries as the world is reminded yet again that health is an interconnected proposition.”
Monkeypox typically kills fewer than 10 percent of people who contract it. At least one person has died in the global outbreak.
As case numbers climb, researchers are working to decipher the genetic blueprint of the virus, in hopes of uncovering whether some viral mutations might explain why the virus has quickly gained a foothold in new places.
Tracing the mutations
The closest known relative of the versions of the virus behind the global outbreak comes from Nigeria, hinting that the outbreak may have got its start there.
In the newest surge in cases, scientists have uncovered more viral changes than anticipated — a sign that the virus may have been circulating undetected among people for a while, perhaps since Nigeria’s 2017–2018 monkeypox outbreak, new research suggests. What’s more, a group of enzymes known for their virus-fighting abilities in the body may be to blame for many of those mutations.
A genetic analysis of monkeypox viruses involved in the global outbreak from 15 people across seven countries shows that these viruses have an average of 50 more genetic tweaks than versions circulating in 2018 and 2019, researchers report June 24 in Nature Medicine. That’s roughly six to 12 times as many mutations as scientists would have expected the virus to develop over that time. Unlike some other types of viruses, poxviruses, which include smallpox and monkeypox viruses, typically mutate fairly slowly.
The changes have a pattern that is a hallmark of an enzyme family called APOBEC3, the researchers say. These enzymes edit DNA’s building blocks — represented by the letters G, C, A and T — in a specific way: Gs change to As and Cs to Ts. The analysis found that particular pattern in the viral sequences, suggesting that APOBEC3s are responsible for the mutations.
Ideally, so many DNA building blocks are swapped for another that a virus is effectively destroyed and can’t infect more cells. But, sometimes, APOBEC3 enzymes don’t make enough changes to knock out the virus. Such mutated, though still functional, viruses can go on to infect additional cells, and possibly another person.
A big question, though, is whether the genetic tweaks seen in the monkeypox virus are helpful, harmful or have no effect at all on the virus.
While it’s still unknown whether the enzymes are directly responsible for the changes in the monkeypox virus, similar mutations are still popping up, the team found. So, APOBEC3s may still be helping the virus change as it continues to spread. One member of the enzyme family is found in skin cells, where people with monkeypox can develop infectious pox lesions.

Different symptoms
Symptoms reported in the global outbreak have been generally milder than those reported in previous outbreaks, perhaps allowing the disease to spread before a person knows they’re infected.
It is not clear whether those differences in symptoms are related to changes in the virus, Inger Damon, director of the CDC’s Division of High-Consequence Pathogens and Pathology, said June 21 in a news briefing hosted by SciLine, a service for journalists and scientists sponsored by the American Association for the Advancement of Science.
Typically, in previous outbreaks, people would develop flu-like symptoms, including fever, headaches, muscle aches and exhaustion about a week or two after exposure to the virus. Then, one to three days after those symptoms start, a rash including large pus-filled lesions pops up generally starting on the face and limbs, particularly the hands, and spreads over the body. Though generally milder, those symptoms are similar to smallpox, but people with monkeypox also tend to develop swollen lymph nodes.
All patients in the U.S. outbreak have gotten rashes, Damon said, “but the lesions have been scattered or localized to a specific body site, rather than diffuse, and have not generally involved the face or the … palms of the hand or the soles of the feet.” Instead, rashes may start in the genital or anal area where they can be mistaken for sexually transmitted diseases, such as syphilis or herpes, she said.
In many cases, the rashes have not spread to other parts of the body. And the classical early symptoms such as fever have been “mild and sometimes nonexistent before a rash appears,” Damon said.
Monkeypox is transmitted from person to person through close skin-to-skin contact or by contact with contaminated towels, clothes or bedding. It may also be spread by droplets of saliva exchanged during kissing or other intimate contact. The CDC is investigating whether the virus might be spread by semen as well as skin-to-skin contact during sex, Agam Rao, a captain in the U.S. Public Health Service, said June 23 at a meeting of the CDC’s Advisory Committee on Immunization Practices.
“We don’t have any reason to suspect it is spread any other way,” such as through the air, Rao said.
In Nigeria, more monkeypox cases have been recorded among women, while the global outbreak has affected mainly men, particularly men who have sex with men. Experts warn that anyone can be infected with monkeypox, and some people face an increased risk of severe disease. Those at increased risk include children, people who are immunocompromised, pregnant people and people with eczema.
The risk of catching monkeypox through casual contact is still low in the United States, Rao said. But data she presented show that while people in the country have contracted monkeypox while traveling abroad, cases have also spread locally.







