A new device can detect the coronavirus in the air in minutes
The detector is about as sensitive as a PCR test but quicker
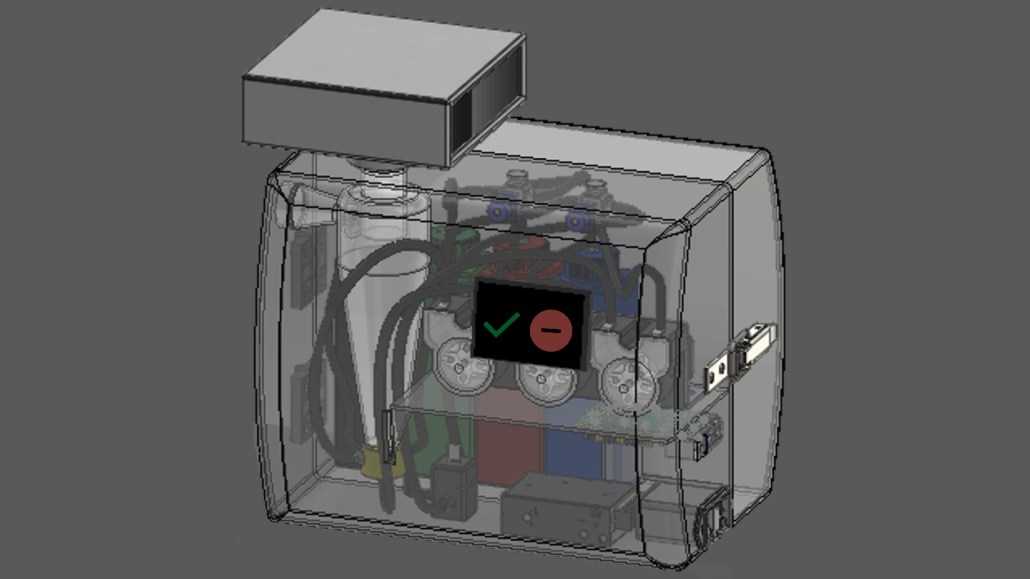
A coronavirus detector (illustrated in a 3-D rendering of a proposed final design) can sense airborne SARS-CoV-2, the virus that causes COVID-19, in just five minutes.
Joseph Puthussery/Washington Univ. in St. Louis
- More than 2 years ago
Read another version of this article at Science News Explores
If you’ve ever thought it would be great to walk into a room and know whether the virus that causes COVID-19 is hanging around, scientists have a device for you. Researchers have created a machine a little bigger than a toaster that can detect airborne SARS-CoV-2 coronavirus in minutes.
It takes only five minutes to detect as few as seven to 35 viral particles per liter of air, researchers report July 10 in Nature Communications. That is about as sensitive as PCR nasal swab tests, says Rajan Chakrabarty, an aerosol scientist at Washington University in St. Louis. His team worked “nonstop” for three years to create the detector, he says.

One of the main challenges when sampling airborne viruses is collecting enough air to concentrate viral particles at detectable levels. Previous attempts have sucked in between 2 and 8 cubic meters of air per minute. This detector pulls in 1,000 cubic meters of air each minute.
To trap the virus, “we create an artificial cyclone inside of the sampler,” Chakrabarty says, by swirling liquid at high speed. Viruses get trapped in the wall of the cyclone and concentrated for analysis. Any viruses not captured in the liquid get filtered out of the air with a HEPA filter attached to the device. After five minutes of collection, the liquid is pumped to a biosensor.
The biosensor consists of an electrode attached to a llama nanobody, a specialized immune system protein made by llamas and their relatives that fights infections much the way antibodies do but is smaller and perhaps tougher than human antibodies (SN: 9/14/20). The nanobody grabs any passing coronavirus by its spike protein. Electricity passing through the nanobody and spike protein causes tyrosine amino acids in the spike protein to oxidize, or lose electrons. Another device attached to the electrode detects that oxidation as a change in voltage, signaling that SARS-CoV-2 is in the air.
The biosensor is based on a detector for the amyloid-beta protein fragments that form Alzheimer’s disease plaques developed by Chakrabarty’s colleagues Carla Yuede and John Cirrito.
To test the detector, the researchers sent the device to the apartments of two people who had COVID-19 infections. “The device was detecting even the trace amounts of virus being shed by the patients,” Chakrabarty says. Air collected from an empty, well-ventilated conference room showed no sign of the virus.
“They’ve demonstrated that it works. It’s able to detect [the] virus at low levels that we would be concerned about in the air,” says Linsey Marr, an aerosol scientist at Virginia Tech in Blacksburg who studies the spread of viruses. She was not involved in the study but is working on a detector, too.
There are still some challenges to overcome. For instance, the device is about as noisy as a vacuum cleaner or a ringing phone. That’s probably too loud to use continuously in a classroom or office, Marr says, but could be tolerated if run for 10 minutes.
Such detectors cost about $1,400 to $1,900 to build in a research lab, Chakrabarty says. Commercial versions may initially be too expensive for home use, Marr says, but could be used in hospitals, airports and other public areas to survey for the virus. The devices could be linked into HVAC systems, which could ramp up ventilation and filtration if the virus is found, Marr and Chakrabarty suggest.
In the future, Chakrabarty hopes to add llama nanobodies that can detect other respiratory viruses as well, such as influenza or respiratory syncytial virus.







