Protein tweak may trigger Alzheimer’s
Unusual version of disease-linked amyloid-beta sows destruction in mouse brains
Scientists have caught tiny amounts of a strangely shaped protein — a relative of a well-known suspect in Alzheimer’s disease — spreading destruction throughout the brains of mice. If a similar process happens in the human brain, it could help explain how Alzheimer’s starts, and even suggest new ways to stop the dangerous molecule’s spread.
Many Alzheimer’s researchers believe the abundance of a molecule called A-beta in the brain is one of the key steps in developing the disease. A-beta commonly takes the form of a chain of 42 protein building blocks called amino acids.
The new study chronicles the dangers of a modified A-beta that lacks the first two amino acids in the chain. Capping this stub is a rare, circular amino acid called pyroglutamate. Until recently, this form “has been largely ignored as some minor mysterious form of amyloid-beta,” says study coauthor George Bloom of the University of Virginia. Yet even trace amounts of this version, called pyroglutamylated A-beta, or pE A-beta, are devastating to mouse nerve cells, he and colleagues report online May 2 in Nature.
“This opens up a whole new view of the disease,” says neurogeneticist Rudy Tanzi of Harvard Medical School. Instead of focusing just on the amount of A-beta in the brain, scientists need to pay attention to modifications of the molecule, too, he says.
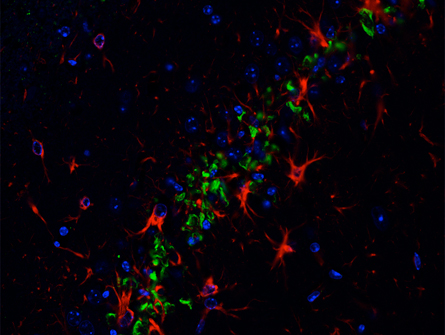
Minuscule amounts of pE A-beta can pair up with more commonplace types and trigger them to misfold, the team reports. These misfolded molecules are then much more deadly to nerve cells, killing about half of mice nerve cells tested in a dish within 24 hours. Experiments with pE A-beta in the brains of mice revealed signs of massive damage, too. “Even at vanishingly small quantities, the mixture is still toxic,” Bloom says.
But this toxicity required a co-conspirator — a protein called tau that tangles up inside nerve cells. Mice genetically designed to lack tau were largely immune to the ill effects of pE A-beta, the team reports. Scientists don’t yet understand exactly how tau and A-beta interact.
It’s not clear whether the results in mice will apply to people. Bloom and his colleagues detected pE A-beta in three out of three postmortem brains of people diagnosed with Alzheimer’s, and one out of three from people without the disease.
The study may have uncovered one of the first steps in a long disease process, says Tanzi. “This puts even more emphasis on early detection of the disease before symptoms appear,” he says. “We really need to hit this disease early.”
The research also points out one potential new way to do that. A Germany-based company called Probiodrug, where three coauthors of the study work, is developing a medicine designed to curb pE A-beta’s production in the brain by targeting the molecule’s creator — an enzyme called glutaminyl cyclase. In 2011, the company announced positive results from preliminary safety tests of the drug in healthy volunteers.







