A second HIV patient has gone into remission after a stem cell transplant
The stem cells came from a donor unable to make a protein needed by the deadly virus
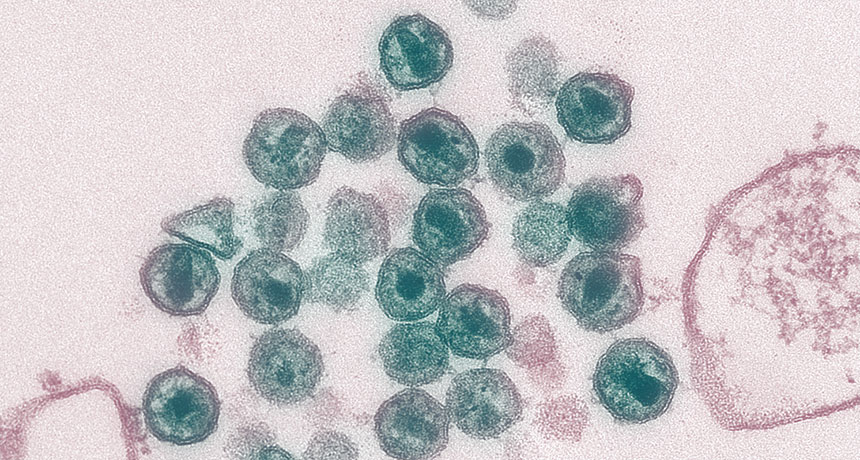
NO ENTRY HIV needs two surface proteins to enter into immune cells called T cells and replicate. An HIV patient went into remission after getting a stem cell transplant with cells that can’t make one of those surface proteins.
Maureen Metcalfe, Tom Hodge/CDC
For only the second time in recorded medical history, a man’s HIV infection has gone into remission.
The patient — positive for the virus that causes AIDS since 2003 — had received a blood stem cell transplant in 2016 as treatment for Hodgkin’s lymphoma, a cancer of the lymphatic system. The blood stem cells came from a donor with a mutation that makes cells resistant to an HIV infection.
Subsequent testing over 12 months showed the patient’s HIV had fallen to undetectable levels. So 16 months after the procedure, the patient stopped taking antiretroviral medication under medical supervision. He has remained in remission ever since, with HIV levels measuring less than one copy per milliliter of plasma, researchers report online in Nature March 5.
Although it’s too early to call the patient cured, “it’s pointing in that direction,” says coauthor Ravindra Gupta, an infectious disease specialist at the University of Cambridge.
Nearly 37 million people worldwide were living with HIV in 2017, with 1.8 million people newly infected that year, according to UNAIDS. Antiretroviral therapy, or ART, has helped many patients live longer by reducing virus levels in the blood, but the drugs need to be taken for life.
During an HIV infection, the virus ambushes immune cells called T cells and makes copies of itself. To enter the T cell, HIV first binds to a cell surface protein called CD4 and then grabs onto another surface protein. Most HIV binds to one called CCR5, although some HIV variants grab one called CXCR4 — or are capable of using either protein.
Once it was clear that the patient, who has chosen to remain anonymous, would undergo a stem cell transplant for Hodgkin’s lymphoma, physicians were able to locate a donor with a defect in both copies of the CCR5 gene. That meant the donor’s T cells couldn’t make the CCR5 protein. And without this protein, most HIV variants can’t get into the cells. The doctors determined that the patient had CCR5-using HIV, and so they suspected — correctly — that the transplant might halt the HIV infection.
The case provides “solid evidence for remission,” says Hans-Peter Kiem, a physician who studies cell and gene therapy at the Fred Hutchinson Cancer Research Center in Seattle, and was not involved in the research. The “only way to tell whether [this is a] long-term remission or cure is longer follow-up.”
The first case to hint that an HIV cure may be possible was reported in 2009 in the New England Journal of Medicine. That case involved the “Berlin patient,” later identified as Timothy Ray Brown, who had undergone a cancer treatment that was similar to but more severe than what the patient in the Nature study received. Having a second person in remission means the first case “wasn’t a chance event,” Gupta says.
Brown’s cancer treatment included two blood stem cell transplants from a donor with a defect in both copies of the CCR5 gene along with two rounds of full body irradiation. The second patient had chemotherapy and only one stem cell transplant.
While these transplants appear to be effective at stopping HIV, they are not an option for most HIV patients. Naturally having the defect in both copies of the CCR5 gene is very rare and is more likely in those of Caucasian descent, making it extremely difficult to find transplant matches for most people.
Another approach may be to manipulate the ability of a patient’s own T cells to make the CCR5 protein, and there are clinical trials under way in the United States testing different methods of preventing CCR5 from functioning in patients. “We need to learn how to make this work” with a patient’s own cells in order for the approach to be available more widely, Kiem says.







