Ultrasound allows a chemotherapy drug to enter the human brain
An early-stage clinical trial shows promise for people with a treatment-resistant brain cancer
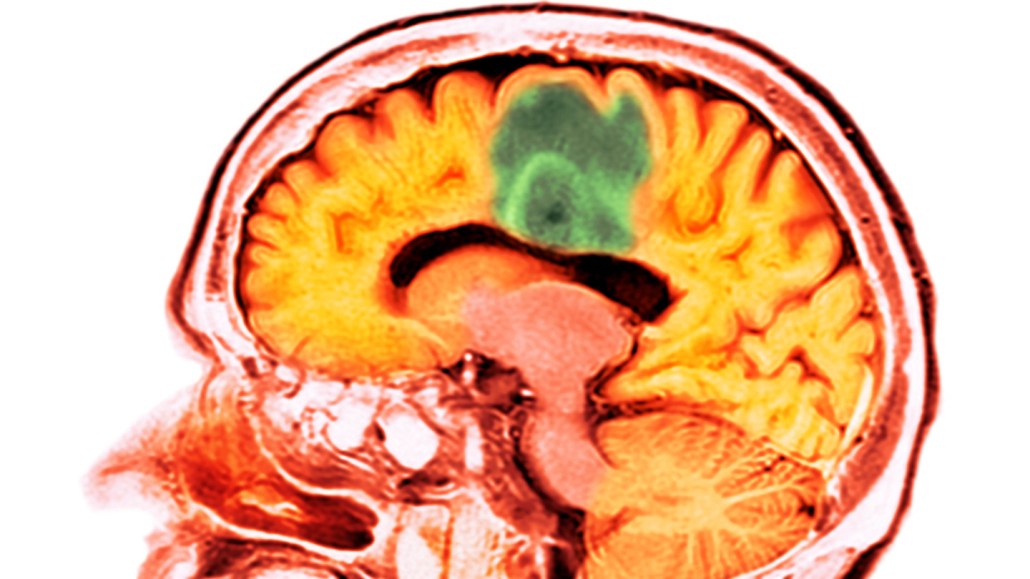
Glioblastoma (green in this CT scan) is a type of brain cancer that is difficult to treat. A study shows how pairing ultrasound with microbubbles temporarily opens the brain’s protective barrier, allowing a chemotherapy drug to enter the organ.
DR P. MARAZZI/SCIENCE PHOTO LIBRARY/Getty Images
Cracking the code to brain cancer treatment might start with cracking the brain’s protective shield.
Nearly impenetrable walls of jam-packed cells line most of the brain’s blood vessels. Although this blood-brain barrier protects the organ from harmful invaders, it also prevents many medications from reaching the brain.
Now, scientists can get a powerful chemotherapy drug into the human brain by temporarily opening its protective shield with ultrasound and tiny bubbles. The early-stage clinical trial, described May 2 in the Lancet Oncology, could lead to new treatments for those with brain cancer.
Better treatments are especially needed for glioblastoma, a common and aggressive type of brain tumor. Even after surgical removal, another mass tends to grow in its place.
“There’s really no established treatment for when the tumors come back,” says neurosurgeon Adam Sonabend of the Northwestern University Feinberg School of Medicine in Chicago. Patients with recurrent glioblastomas “don’t have any meaningful therapeutic options, so we were exploring new ways of treating them.”
After the initial tumor has been removed, patients typically receive a relatively weak chemotherapy drug that can bypass the brain’s barricade. More potent drugs could help destroy any lingering disease — if the medicines could break through the barrier.
Sonabend and colleagues turned to an exploratory method using ultrasound that has already succeeded at briefly opening the blood-brain barrier in humans (SN: 11/11/15). A person first receives an intravenous injection of a fluid brimming with microscopic bubbles, which fill the body’s blood vessels. This technique is already routinely used to help visualize vessels in ultrasound imaging. In the targeted brain area, ultrasound waves shake the microbubbles, prying open the densely packed blood vessel walls.
To examine safety and dosing of this delivery method and drug, 17 people had their regrown tumor removed and an ultrasound device implanted in their skull, adjacent to the remaining cavity. Patients then received between two and six rounds of treatment spaced three weeks apart.
During each session, participants were injected with microbubbles for 30 seconds and simultaneously received pulses of ultrasound waves for nearly five minutes. The waves reached a specific area of the brain encompassing the tumor cavity, penetrating nearly 8 centimeters deep. That was followed by a 30-minute intravenous infusion of paclitaxel, a potent drug used to treat lung, breast and other cancers. It typically can’t access the brain.
In the brain tissue zapped by ultrasound, researchers found nearly four times as much paclitaxel compared with tissue outside of range. MRI scans and a special dye revealed that the blood-brain barrier mostly closed back up within 60 minutes.
Overall, paclitaxel and the delivery method were well tolerated up to the maximum tested drug dose of 260 milligrams per square meter, the dose approved by the U.S. Food and Drug Administration for breast cancer. Some patients, however, reported temporary side effects including headaches and confusion.
“This definitely is a very interesting paradigm that can be applied not just to glioblastoma but other brain tumors,” says pediatric radiation oncologist Cheng-Chia Wu of the Columbia University Irving Medical Center in New York City who was not involved in the work. It “creates a whole host of opportunities.”
Although this early-stage clinical trial offers a glimmer of hope, Wu points out that it will take time to continue testing this potential treatment. But one day it could help extend glioblastoma patients’ life spans following diagnosis, which average a little over a year.
For now, Wu says, “this is definitely a very good first step in the right direction.”







