Antibiotics might fight Alzheimer’s plaques
Mouse study links drug-induced changes in gut bacteria to reduced A-beta buildup in brain
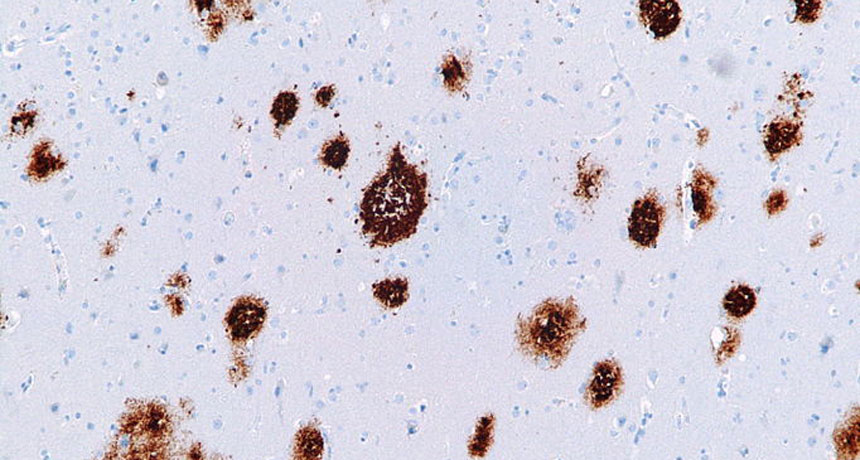
PLAQUE FIGHTER A long dose of antibiotics reduced Alzheimer’s-related plaques (shown here in a human brain) in the brains of mice, results that suggest gut bacteria can influence the disease.
Nephron/ Wikimedia Commons (CC BY-SA 3.0)







