Bioengineering better blood vessels
Durable conduits made by living cells might boost options for dialysis, heart bypass patients
Using human cells as tiny factories, researchers can grow new blood vessels that might someday provide a valuable option for patients undergoing surgery for kidney dialysis or a heart bypass. The new study testing the bioengineered vessels in baboons and dogs raises the prospect of mass-producing such natural-tissue vessels, researchers report in the Feb. 2 Science Translational Medicine.
In coronary bypass surgery, a vein is typically stripped out of a part of the body that can manage without it and implanted on the heart as a conduit supplying blood to the heart muscle. But in some patients, vessels are inaccessible due to obesity, deterioration or having been used up in other operations. Those individuals have few alternatives beyond medication, says study coauthor Alan Kypson, a surgeon at East Carolina University School of Medicine in Greenville. “A blood vessel that comes right off the shelf for a bypass — that’s potentially groundbreaking stuff,” he says.
The first population to benefit from these bioengineered vessels would probably be kidney failure patients who need to undergo dialysis, in which the blood is cleansed every few days. Dialysis needs fast blood flow to work well, so a patient’s best option is surgery to join a large artery directly to a vein, creating a circulatory shortcut that provides an area of surging blood and facilitates dialysis. But many patients have vessels unfit for that surgery or the surgery does not succeed, so they often get implanted with a synthetic vessel to join an artery and vein. Both operations, typically done in an arm, carry risks of infection and clogging from a buildup of cells.
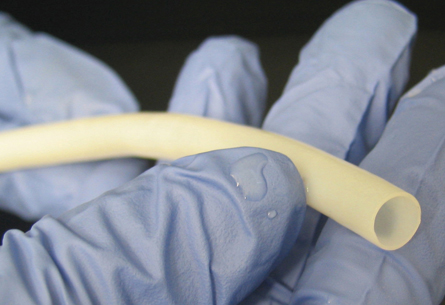
In the new study, Kypson and his colleagues tested large bioengineered vessels in baboons. To make the vessels, the scientists cultured smooth muscle cells obtained from human blood vessels on a biodegradable tube of micromesh similar to material used in dissolvable sutures. After the cells had built a vessel by depositing collagen and other compounds on the mesh, the scientists removed the cells to leave behind a vessel of tough human proteins. Removing the living cells discourages immune attack on the vessels and also allows them to be stored in refrigerators for up to a year, says study coauthor Shannon Dahl, a biomedical engineer at Humacyte in Durham, N.C.
The vessels were tested for suture strength, stretchiness and ability to withstand pressure. “If you’re going to grow blood vessels, you have to make sure they won’t burst,” Kypson says.
The researchers implanted these bioengineered vessels into baboons in the same way synthetic vessels are grafted into dialysis patients. The vessels showed little evidence of clotting and cell buildup even after six months, the longest large-animal test of a tissue-engineered vessel grown in a lab, Dahl says.
Implants for dialysis are large by vessel standards, nearly 1 centimeter in diameter. The researchers also grew vessels one-third that size, 3 millimeters, for heart bypass experiments in dogs. Those vessels were “seeded” inside with natural vessel-lining cells called endothelial cells. These cells release anticlotting factors that promote blood flow, says study coauthor Laura Niklason, an anesthesiologist and tissue engineer at Yale University School of Medicine. This function kept blood moving in the month-long test in the dogs.
In people, a vessel recipient would donate his or her own endothelial cells for placement in a bioengineered vessel, which would delay surgery only a few weeks, the researchers say.
“Vascular access is known as the Achilles heel of dialysis,” says epidemiologist Paul Eggers of the National Institute of Diabetes and Digestive and Kidney Diseases in Bethesda, Md. “Keeping the vascular site open is big deal.” He notes that several lines of bioengineering are under way, and this process seems to land halfway between surgically connecting an artery with a vein and installing a synthetic graft in the arm. “It may turn out to be a wonderful thing. This looks like something one should keep an eye on.”
The team is preparing an application to test the technology in people with dialysis “in about a year,” Niklason says.
Bioengineered blood vessels from Science News on Vimeo.
A narrated video briefly explains how replacement blood vessels are created and used.
Credit: Video © Science/AAAS







