Why a popular breast cancer drug may be less effective for some Africans
A gene mutation appears to impair tamoxifen’s ability to tackle the disease
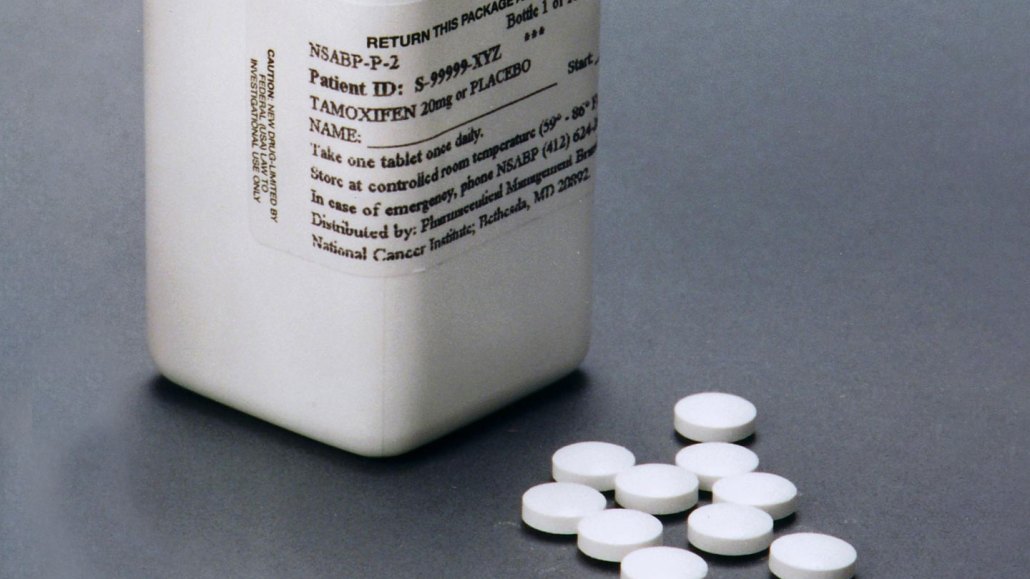
Tamoxifen, a breast cancer drug, helps derail a strategy that cancer cells exploit to grow.
Bill Branson/National Cancer Institute
WASHINGTON — A genetic variant commonly found in some Africans may stymie the effects of a popular breast cancer drug.
The variant produces a sluggish version of the enzyme known to activate tamoxifen. People who inherit two copies of the variant show five times less active drug in their bloodstreams compared with people who don’t have that variant, researchers reported November 2 at the American Society of Human Genetics annual meeting. As a result, many of these patients may receive a dose that’s insufficient to treat their cancer.
The gene, called CYP2D6, that produces the crucial enzyme differs dramatically among people. On average, a fifth of Africans carry at least one copy of the variant that the researchers studied. Across the continent, however, that figure ranges from a slim 5 percent to over 34 percent.
Preemptive genetic screening that identifies patients with the genetic variant would probably cost too much for local clinics and hospitals, says molecular geneticist Comfort Kanji, who is based at the African Institute of Biomedical Science and Technology in Harare, Zimbabwe. But he imagines that his team’s findings could inspire clinical trials that test larger starting doses of tamoxifen in heavily affected groups.
Kanji and his colleagues collected daily blood samples from 42 Zimbabweans taking tamoxifen. Some of the participants had one copy of the variant, while others had two. A third group had a different version of the gene with no known effect on the enzyme. The differences in how they metabolized the medication emerged right away and remained for the duration of the 3-week-long experiment.
Additionally, simulations suggested that doubling the prescribed amount of the drug for participants with two copies of the variant would bring levels of active drug in the blood back to normal — and with few short-term consequences.
The study provides powerful results despite a small sample size, says David Twesigomwe, a pharmacogeneticist at the Sydney Brenner Institute for Molecular Bioscience in Johannesburg who was not involved in the research.
It offers a clear-cut case for metabolic screening, he says. Even as comprehensive genetic testing remains out of reach for many Africans, he believes simpler, narrower tests could do the trick, potentially laying the foundation for clinicians to incorporate screening more widely in treatment.
Each year, around 200,000 people in sub-Saharan Africa receive diagnoses of breast cancer. Roughly 40 percent survive for longer than five years past their diagnosis, unlike 86 percent in the United States. The main reason is that many patients in Africa struggle to access or afford treatment, and as a result, show up to clinics with late-stage cancers. This new finding is unlikely to turn those cases around, but it could help make timely care more effective, Kanji says.
Worldwide, about 30 percent of patients with estrogen receptor-positive breast cancer — the most common type — show little improvement on tamoxifen. That proportion is even higher among African women, Kanji says. The prevalence of the studied gene variant, or others with a similar effect, could offer a partial explanation.
A separate study would be required to see if the findings extend to African Americans, Kanji and Twesigomwe both say. In the United States, Black women are 40 percent more likely to die of breast cancer— with about 28 deaths per 100,000 for Black women compared with 20 per 100,000 for white women — despite a similar rate of diagnosis.
Experts caution that the reasons why are multifaceted, including biological, sociological and historical. The role that a variant of CYP2D6 plays may constitute a sliver of a sliver.
The enzyme that the gene generates metabolizes more than just tamoxifen. It’s responsible for breaking down many other drugs, including opioids, beta-blockers and a common class of antidepressant drugs called selective serotonin reuptake inhibitors. That means that people with different variants of the gene may respond better or worse to those medications too.







