Millions of COVID-19 cases in the U.S. may have gone undiagnosed in March
A surge of flulike illnesses suggests the virus was already much more widespread than thought
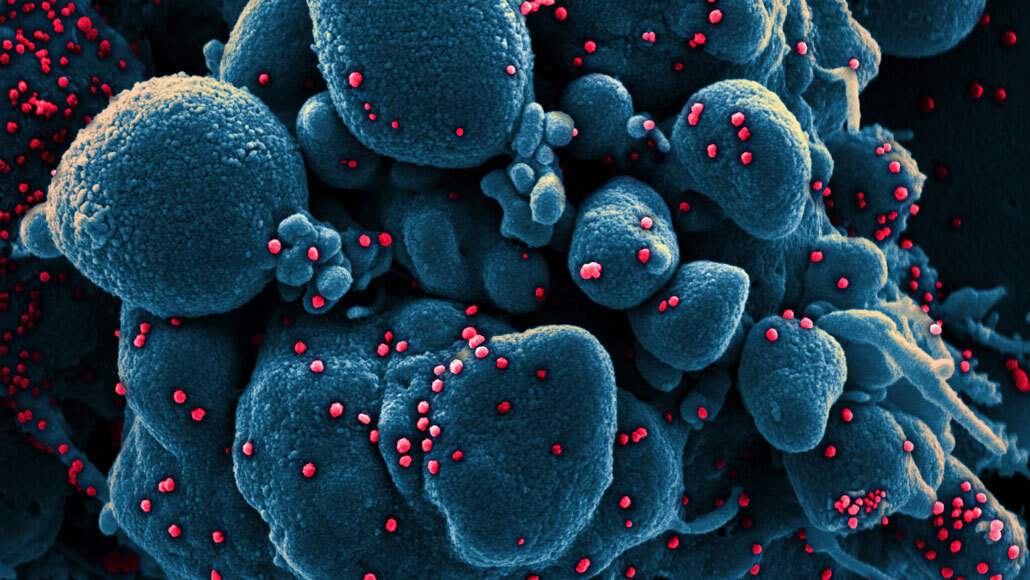
The coronavirus, shown (red) infecting a dying cell (blue) in this colorized scanning electron micrograph, may have infected more than 8.7 million people in the United States during three weeks in March, researchers estimate from data on doctor’s office visits for influenza-like illnesses.
NIAID
The United States may have had millions more COVID-19 cases in March than previously thought.
More than 8.7 million people may have contracted the coronavirus from March 8 to March 28, but more than 80 percent of them were never diagnosed with COVID-19, researchers report June 22 in Science Translational Medicine. Officially, the country has recorded more than 2.3 million COVID-19 cases since January, and more than 9.4 million cases have been reported worldwide since December.
The estimate was made using data gleaned from a network that monitors influenza-like illnesses in United States. That network, ILINet, was set up to give public health officials a way to track flu outbreaks. Doctors in some offices across the country report to the Centers for Disease Control and Prevention when patients come in with flulike symptoms, including results of flu tests. Researchers can extrapolate from there what is happening in the rest of the state or country. But the data can also be used to track other respiratory viruses, says Justin Silverman, a physician and statistician at Penn State.
In early February, Silverman’s colleague, Alex Washburne, a mathematical epidemiologist at Montana State University in Bozeman, realized that the number of coronavirus cases was doubling faster than expected. So he, Silverman and Nathaniel Hupert, an internal medicine doctor at Weill Cornell Medicine in New York City, began watching the data on flulike illnesses to see if that information could indicate that the epidemic was taking off in the United States (SN: 2/28/20).
In March, a surge in influenza-like illnesses arose, exactly as the researchers expected. In some places, the surge was huge. In New York, for instance, twice as many influenza-like illnesses that weren’t due to flu were recorded in March than had ever been seen in the 10 years since the network’s inception.
Subtracting out influenza and the expected number of seasonal cases of other flulike illnesses left the researchers with a large number of unexplained illnesses in the country that could be due to SARS-CoV-2, the virus that causes COVID-19.
Assuming that only a third of people infected with the coronavirus go to the doctor (based on extrapolations from how many people with mild symptoms go to hospital emergency rooms and figuring in rates of people who are infected but don’t have symptoms), those excess cases would correspond to more than 8.7 million COVID-19 cases nationwide during the three-week study period, the team estimates. About 120,000 confirmed cases of COVID-19 had been reported in the country as of March 28.
“It’s a staggering result,” Silverman says. “I remember calling Alex and saying, ‘This can’t possibly be right. We must have made a mistake somewhere.’”

Trustworthy journalism comes at a price.
Scientists and journalists share a core belief in questioning, observing and verifying to reach the truth. Science News reports on crucial research and discovery across science disciplines. We need your financial support to make it happen – every contribution makes a difference.
But Washburne pointed out that their calculations of the fast growth of the epidemic were in line with that number. Also, states with extra influenza-like cases also had higher COVID-19 case counts. “That gave us additional evidence to suspect that this surge in visits could be COVID,” Washburne says.
“That’s when we started believing that this wasn’t just a math error,” Silverman says.
Antibody tests in mid-April indicated that almost 14 percent of people tested in New York state had antibodies against the virus, governor Andrew Cuomo announced in a news conference on April 23. That number suggests that coronavirus infections were already widespread in the state, and are in line with their estimates, the researchers say.
Robert Redfield, director of the U.S. Centers for Disease Control and Prevention, said June 25 in a call with reporters that the agency estimates that for every case that’s been reported, there are actually 10 other infections in the country, based on antibody test results.
“It seems possible or likely that ‘surges’ of [influenza-like illnesses] may be an indication of a surge in SARS-CoV-2 and could provide some useful signals,” says Roger Chou, an internal medicine doctor at Oregon Health & Science University in Portland not involved in the work.
But the study makes several assumptions that may not be correct, Chou says. For instance, many of the excess flulike illness, “are not necessarily SARS-CoV-2 — just people seeking care when they wouldn’t in a normal year,” he says. Changes in testing rates (SN: 3/6/20), doctors switching to televisits and other changes to health care this spring can make it very hard to interpret the surveillance data, Chou says.
Another assumption is that the clinics reporting results to the network are just like clinics elsewhere in the state or country, which probably isn’t the case, says Arthur Reingold, an epidemiologist at the University of California, Berkeley School of Public Health. “Can you extrapolate from Santa Clara County [in California] to Montana … or from a study done in the Boston area to Charleston, South Carolina? Probably not.”
Surveillance can alert authorities of when an outbreak gets going and is starting to subside, but aren’t as good for determining how large the outbreak is, Reingold says. Direct testing for coronavirus infections is more likely to give a handle on the size of the epidemic going forward (SN: 4/17/20), especially since most ILINet clinics report cases only during flu season between September and early April.







