These tiny aquatic animals secrete a compound that may help fight snail fever
A molecule made by rotifers prevents parasitic worm larvae from causing infections in mice
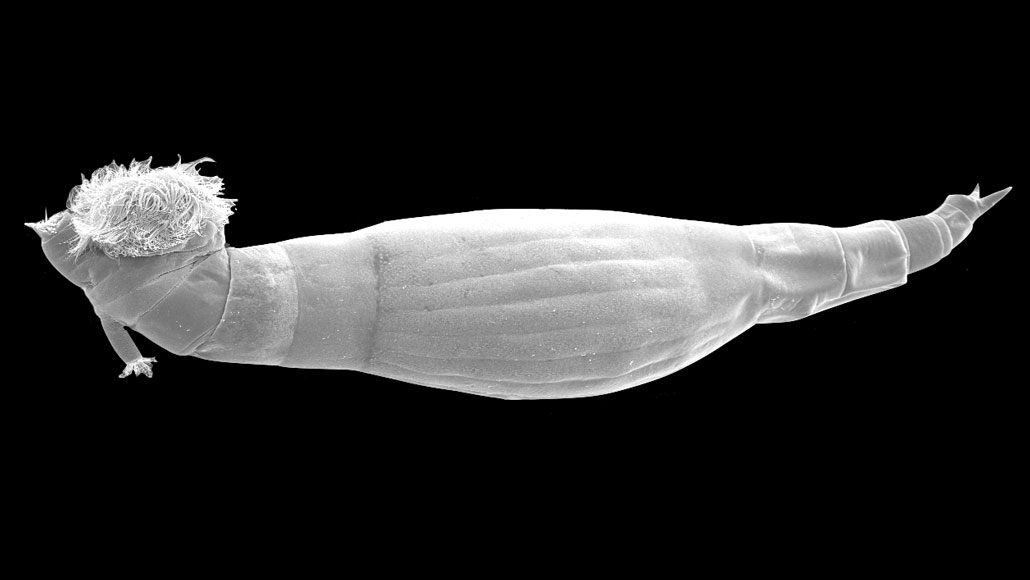
The rotifer Rotaria rotatoria (shown in a microscope image) produces a newly identified molecule that paralyzes the larvae of worms that cause schistosomiasis, preventing them from spurring new infections.
Newmark Lab
Tiny aquatic invertebrates, once a nuisance to scientists studying snail fever, may actually hold the key to fighting the spread of the tropical disease.
Snail fever, or schistosomiasis, is caused by several species of freshwater parasitic worms that penetrate human skin to enter the bloodstream. The parasites must first infect aquatic snails before developing into larvae, the life cycle stage that can infect people. For decades, scientists studied the parasites as they infested snails, and grew frustrated when specimens were contaminated by microscopic invertebrates called rotifers. Somehow, the presence of rotifers paralyzed the larvae, preventing them from infecting other organisms.
Now, scientists have identified a molecule secreted by rotifers that causes the paralysis. Larvae of Schistosoma mansoni worms, a type of schistosome or blood fluke, became paralyzed within 30 seconds of being submerged in water containing the molecule in tiny quantities. Paralyzed larvae in rotifer-contaminated water also could not infect mice whose tails were placed in the same water for half an hour, the team reports October 17 in PLOS Biology.
The researchers “have taken what was considered kind of a nuisance for people who work with schistosomes … and used it to come up with a really novel, interesting finding,” says Robert Greenberg, a parasitologist at the University of Pennsylvania School of Veterinary Medicine who was not involved in the work.
S. mansoni is one of 10 worm species that can cause schistosomiasis, which affects more than 200 million people worldwide. S. mansoni mostly affects people in tropical regions of Africa, the Middle East, South America and the Caribbean. Left untreated, disease caused by this species can lead to fever, chronic liver damage, abdominal pain, anemia or leaky blood vessels. The worms live inside blood vessels, feasting on proteins (SN: 1/10/07) and laying eggs that then hatch and travel through the bloodstream. Many of the eggs end up in the liver — where they cause inflammation — while some are excreted in feces. Other people can then become infected by coming into contact with water contaminated by those feces.
In the new study, researchers allowed the rotifer species Rotaria rotatoria to grow on shells of submerged aquatic snails (SN: 7/21/16). When S. mansoni larvae were placed in the same water, the larvae couldn’t move, suggesting that the rotifers were secreting something into the water that caused the paralysis. The team then tested which molecules in the water caused paralysis, and found only one, which they named schistosome paralysis factor, or SPF.
Mice exposed for 30 minutes to worm-infested water without SPF picked up an average of 83 worms, and the livers of those mice showed deep holes where schistosome eggs had embedded. But when the same water contained a small amount of the molecule, exposed mice didn’t pick up any worms, and their livers looked normal.
It’s unclear how the molecule causes the paralysis, or why rotifers have developed it. But further study of the compound, part of which resembles the neurotransmitter serotonin, may lead to new ways of treating or preventing schistosomiasis. “Hopefully, we can come up with ways to prevent people from getting infected,” says study coauthor and developmental biologist Phil Newmark, a Howard Hughes Medical Institute investigator at the University of Wisconsin–Madison.
Currently, the anti-worm medication called praziquantel used to treat the disease kills adult parasites, but not larvae. Some researchers have also voiced concern about possible drug resistance, evidence of which has emerged in lab experiments. “Identifying new targets and molecules is essential to ensure we have new drugs in the pipeline,” says Jonathan Marchant, a cell biologist at the Medical College of Wisconsin in Milwaukee who was not involved in the study.
The new study illustrates, once again, how chemicals made by animals and plants have the power to supplement human medicine, Marchant says. “It’s an important reminder of the power of nature’s synthetic arsenal.”







