Using checklist reduces surgery complications
WHO guidelines map everything from patient identity to post-operation inventory of sponges
By reading through a list of procedures aloud and checking them off before and after an operation, hospital surgical teams reduce patient complications by more than one-third, a new study finds. In low-income countries, using the checklist also seems to halve in-hospital deaths due to these complications, an international group of scientists reports in a study published online January 14 by the New England Journal of Medicine.
Results from investigations since the 1990s into medical errors spurred the World Health Organization in 2008 to release a checklist designed to limit surgical complications. In the new study, researchers analyzed complication rates in surgical patients at eight hospitals before and after operating teams began using the checklist.
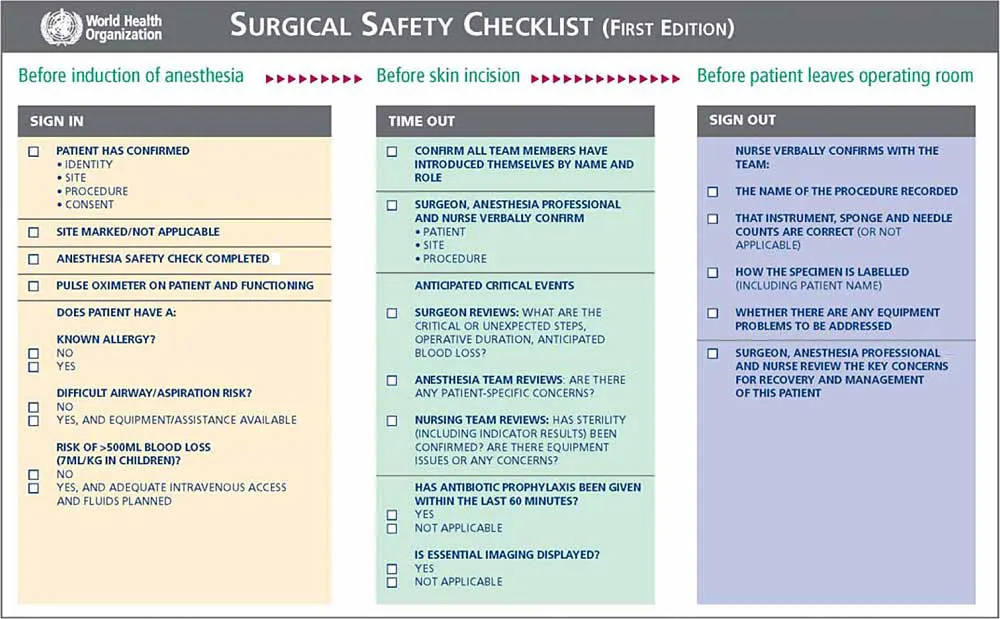
The WHO checklist includes such items as verifying the patient’s identity and surgery site before anesthesia, reviewing the use of antibiotics and the key surgical steps before the first cut, and accounting for all instruments and sponges afterward.
“Surgical care in any hospital is complex and chaotic,” says anesthesiologist Alex Macario of Stanford University, who did not participate in the study. “Checklists help ensure that everyone is on the same page.” Even so, the use of checklists isn’t typically taught in medical schools, he says. “And it is a big cultural change to adopt them consistently at any facility.”
While the use of such surgical checklists appears to be on the rise, their prevalence is unknown.
In the new study, researchers documented any in-hospital complications occurring in 3,733 patients at major hospitals in four low-income countries — India, Tanzania, Jordan and the Philippines — and in four higher-income countries — the United States, Britain, New Zealand and Canada. Roughly half of the patients at each site underwent surgery before the checklist was in use, and half got surgery with a checklist being read aloud in the room.
Complications occurred in 11 percent of patients getting surgery by teams operating without a checklist, compared with only 7 percent of patients whose operating team used one.
Checklist use halved death rates, from 2 to 1 percent, in the low-income countries. Death rates in high-income countries didn’t change substantially with implementation of the checklist.
Procedure checklists are used by crews on airplanes and submarines and at nuclear power plants, points out study coauthor Alex Haynes, a surgeon and researcher at the Harvard School of Public Health and Massachusetts General Hospital in Boston. But he cautions that the surgical checklist “isn’t just a piece of paper. It’s a team exercise involving verbalization of performance and sharing of information.” It’s not that people in operating rooms don’t speak to each other, he says. “But there should be a formal time when this happens.”
Anesthesiologist Peter Pronovost of Johns Hopkins University in Baltimore notes that surgical teams and other professional crews can grow weary of going over procedures. “They call it checklist fatigue,” he says. For that reason, he says, “you have to make sure the elements on the list are relevant to your work area.” So while the WHO guidelines are worth using, some surgeries — such as those involving children or cardiac patients — would require specific entries on a checklist that are not appropriate for other surgeries, he says.
Haynes agrees and points out that the WHO checklist provides a baseline. “It’s quite likely that modifications can and should be made to the checklist for specific environments and situations,” he says.







