A new strategy to rebalance out-of-control immune systems could one day stop autoimmune diseases. The method, tested in mice, preserves the body’s ability to fight off bacteria and viruses.
Autoimmune diseases result when the immune system mistakes some of the body’s proteins for invaders and attacks organs. Doctors usually treat such disorders — including type 1 diabetes, multiple sclerosis, lupus and rheumatoid arthritis —with immune-suppressing drugs. The drugs calm the attacks but damage the ability to fight infections and cancer.
But research now shows that the immune system can relearn that the body’s proteins are friends, not foes. Scientists broke down and rebuilt the immune systems of mice with diseases that mimic type 1 diabetes and MS. The treatment stopped the progress of diabetes in four out of five mice and put animals with a disease similar to MS into remission, the team reports in the June 18 Science Translational Medicine.
The treatment works by depleting the body of faulty immune cells and stimulating the formation of new ones called regulatory T cells, or T-regs. Regulatory T cells are akin to military police that watch over the immune system’s soldier cells to make sure they kill only true foes and don’t damage the body’s own cells with friendly fire, says immunologist WanJun Chen of the National Institute of Dental and Craniofacial Research in Bethesda, Md., who led the study. Autoimmune diseases occur in part because T-regs aren’t doing their job properly.
Chen’s T reg retraining program may allow researchers to fix wayward immune systems instead of just quashing them. “Conceptually, these findings have broken the bottleneck in manipulating T-regs for the treatment of human diseases, especially autoimmune diseases,” he says.
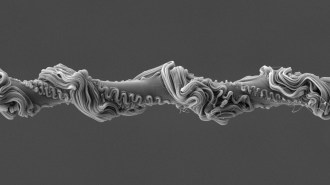
Before new T-regs could form, the researchers had to eliminate old, corrupted immune cells. The team dosed sick mice with enough radiation to cause 60 to 80 percent of their immune cells to commit a form of programmed suicide known as apoptosis. Next, the team injected immune cells called macrophages from the spleens of other mice into the sick animals to gobble up the dying cells. Gorging on dying cells causes macrophages to secrete a chemical called TGF-beta, which stimulates the immune system to produce new T-regs.
To ensure that the new T-regs would prevent autoimmune attacks, the researchers had to program the cells to distinguish self from outsiders. So along with the macrophages, Chen and colleagues injected the mice with the previously attacked body proteins, called autoantigens. The autoantigen boost produced T-regs that were on the lookout for those proteins. When these T-regs found tissues where the autoantigen proteins were made, the cells stopped other immune cells from attacking, Chen says.
The treatment still allowed immune cells to attack bacterial proteins, suggesting that the mice are still able to fend off infectious diseases.
Chen’s team demonstrated that both the macrophages and the autoantigens are necessary for the treatment to work. Irradiated mice lacking either didn’t go into remission from MS.
In other experiments, the researchers demonstrated a way possibly to avoid the radiation step. Antibodies that slate certain immune cells for death can generate enough suicidal cells for macrophages to gorge on. Since the antibodies don’t kill macrophages, the mice had plenty of macrophages to produce the TGF-beta needed to nurture new T-regs. If the technique is ever used to treat humans, antibodies would probably be used instead of radiation, Chen says.
There are still many obstacles to surmount before doctors can use the treatment. It’s not clear whether the body can sustain production of the calming T-regs to provide lasting relief from autoimmune attacks, says immunologist Lucienne Chatenoud of Paris Descartes University in a commentary on the work appearing in the June 20 Science. But if the treatment proves successful in people, she writes, similar techniques may be used to train the immune system to tolerate transplants, gene therapy and engineered tissues.