When Interpol seized an estimated $2.6 million worth of drugs in a blitz last fall, the international crime fighters weren’t after cocaine or heroin. They confiscated thousands of packages of antibiotics, insulin and heart and cancer medications.

The sting, dubbed Operation Pangea III, was part of a less familiar war on drugs — the fight against counterfeit meds. It’s a high-stakes battle: A $1,000 investment in fake drugs can return $30,000, 10 times the typical profit from the same investment in heroin, the U.S. Department of Commerce estimates. This version of drug trafficking also has deadly collateral damage: A 22-year-old woman in Argentina with mild anemia died from liver failure after receiving counterfeit iron injections. More than 50 kids in Nigeria died after taking a teething medication containing the poisonous solvent diethylene glycol. And a Canadian woman died from fake drugs she purchased online; they were loaded with metals, including aluminum, titanium and arsenic.
Counterfeit drugs have long been a problem in regions where the path from manufacturer to consumer is circuitous and full of holes. But the Internet has made it easy for anyone, anywhere, to circumvent legitimate supply chains, taking counterfeit drug trading to new highs — and lows.
Operation Pangea III specifically targeted online drug sales, investigating 694 websites, 297 of which have since been shut down. More than 40 countries participated in the effort, which involved customs officials, the electronic payments industry and the European Heads of Medicines Agencies.
Scientists weren’t lauded in Interpol’s press release. But they played a crucial role in producing key weapons for fighting the counterfeit-drug trade. These tools uncover what can’t be seen with the naked eye — a pill’s ingredients at the scale of molecules or atoms.
While 20th century chemists developed an impressive suite of methods for revealing a substance’s anatomy, in the last decade researchers have developed next-generation versions that simplify the equipment and eliminate tedious sample preparation. New techniques can analyze compounds in seconds, and one recent tweak offers X-ray vision, so a pill’s contents can be assessed without even opening a bottle.
Researchers are also finding ways to construct exquisite maps that show the location of ingredients within a pill, intelligence that may lead inspectors to the source of fakes.
“The scientific community is realizing this is an important problem and we can help,” says analytical chemist Facundo Fernández of Georgia Tech in Atlanta. “It used to be people said, ‘This is a problem for law enforcement.’ Now we’ve started developing new tools, and there is more interest from scientists.”
Spins on spec
Evidence suggests that the fake-drug problem is widespread. Knockoffs include aspirin, antibiotics and drugs for treating heart attacks, hepatitis B and HIV. (Surgical mesh and blood glucose test strips have also been counterfeited.) In the United States and other countries with relatively effective regulatory systems, the proportion of medicines that are fakes is probably less than 1 percent, still a staggering figure considering that more than a billion pills are sold in the United States each year. In countries with less secure supply chains, the problem is worse.
In Cambodia, for instance, a survey of intestinal-parasite drugs found that more than 4 percent were counterfeit, researchers reported last year in Tropical Medicine & International Health. An investigation reported in 2008 that half of malaria drugs collected from parts of Southeast Asia were counterfeit.
When medications contain little to none of the active ingredient, the consequences can be severe. In February 2005, for example, a 23-year-old man arrived at a hospital in Myanmar infected with the malaria parasite. He received pills thought to contain artesunate, the treatment of choice. By the third night he was in a coma and his kidneys had failed; he died soon thereafter.
Infectious-disease specialist Paul Newton of the University of Oxford, who works out of Mahosot Hospital in Laos, and colleagues were called on to figure out what had happened. Analyzing the medication using a technique known as DART-MS revealed that the man’s pills were counterfeit, mostly containing the pain reliever acetaminophen.
The analysis was among the first in which the newly invented DART-MS blew the lid off counterfeit drugs. Short for Direct Analysis in Real Time-Mass Spectrometry, DART-MS is a variant on traditional mass spectrometry, an old analytic technique. At its most basic, mass spec involves vaporizing a sample and electrically charging, or ionizing, the resulting molecules in a vacuum. Those ions are shot through a combination of electric and magnetic fields.
Just as it’s easier to divert the path of a tennis ball than a cannonball, lighter ions (with the same charge) are deflected more than heavier ones. The ions, sorted by their mass-to-charge ratios, pass through a detector. Computer analyses yield a chemical bar code, or spectrum, that reveals a sample’s makeup when compared with a library of the spectra of different elements and compounds. It’s like putting a piece of cake through a machine to find out the precise recipe.
Though traditional mass spec is powerful, a sample has to be carefully prepared to facilitate molecule separation, the analysis has to be done in a vacuum and testing one sample can take 30 minutes. DART-MS and another new twist on mass spec, known as DESI-MS, can reveal a drug’s constituents and relative amounts in seconds, with no sample prep and in open air. People had always assumed that charged particles outside the safety of a vacuum would be too unstable for analysis, immediately getting swept up in a frenzy of reactions.
“Really revolutionary was the realization that … ions are perfectly ordinary stable species and you can move them around in air,” says R. Graham Cooks of Purdue University in West Lafayette, Ind., father of DESI. “It’s still a surprise to some people.”
DART uses plasma and heated gas to turn the sample’s molecules into ions, whereas DESI (short for Desorption Electrospray Ionization) sprays a liquid solvent that ionizes the sample and then evaporates away, leaving the ions behind. Both have become favorite analytical tools, and not just among those investigating counterfeit drugs. DESI, for example, is helping researchers detect explosives, chemical warfare agents, industrial polymers and proteins.
The late John Fenn, a chemist who shared a Nobel Prize for developing the mass spec technique on which DESI is based, was quoted as calling DESI-MS “the greatest thing since night baseball.”
A newer version of DESI, reported by Cooks’ lab in 2006, dopes the stream of solvent with additional molecules that can grab onto ingredients of interest, revealing their presence with much greater sensitivity. Reporting in Analytical Chemistry in 2007, Fernández and colleagues found that “reactive DESI” was 170 times more sensitive than DESI at detecting artesunate in antimalarial meds. In some fakes, the technique also revealed a cheap and less effective chemical relative of the real antimalarial active ingredient.
“Reactive DESI is one of the stars,” Fernández says. “It’s very dynamic. You can use it to selectively detect certain molecules and even quantify them. And you can do it on the fly.”
The method also proved useful for screening Tamiflu, fake versions of which sold widely on the Internet during recent flu outbreaks.
Tickled with light
While lack of active ingredients means that a patient isn’t getting the expected benefit, the wrong ingredients can result in symptoms that make diagnosis difficult. And in some cases, wayward ingredients can be deadly.
In Singapore in 2008, 149 men were admitted to hospitals with severe low blood sugar; these men were not diabetic, but seven went into comas and four subsequently died. The culprits were various versions of fake sexual enhancement and erectile dysfunction drugs contaminated by glyburide, a powerful diabetes drug, scientists reported in the New England Journal of Medicine in 2009.
The embarrassment and high price associated with erectile dysfunction drugs such as Viagra and Cialis, known as phosphodiesterase type 5 inhibitors or PDE5Is, make them among the most commonly purchased over the Internet, a land rife with cons. Since Viagra hit the market in 1998, it has also become one of the most widely counterfeited drugs in the developed world. From 2004 to 2008, 35.8 million fake Viagra tablets were seized in Europe. In Japan, sales of illicit PDE5Is are estimated at 2.5 times larger than the market for genuine counterparts, researchers reported last year in Environmental Health and Preventive Medicine.
In another paper published last year, in the International Journal of Clinical Practice, researchers cited a laundry list of other pharmaceuticals that have turned up in fake erectile dysfunction drugs, including acetaminophen; the ovary-stimulating drug clomiphene; fluoxetine, the active ingredient in Prozac; and dipyrone, an anti-inflammatory used by veterinarians to treat horses. Other ingredients include lactose, talcum powder and printer ink (used to paint the fake little blue pills blue).
In addition to the mass spec techniques, researchers are tickling medications with light to betray unwanted components. Light can offer a spectral readout without destroying the compound — an important consideration for patients who want to take the drug if it’s real and for law enforcement officials who would use a fake as evidence.
One light-tickling technique can analyze bottled samples without opening the bottle. It’s a play on Raman spectroscopy, in which a laser beam set to one wavelength, or color, is shined on a sample. A small number of photons from the beam will send the sample’s molecules oscillating like a spring, emitting light of a different color, which when analyzed yields a chemical bar code.
Normally, shining a laser light on a turbid bottle would just produce a dazzling glare, obscuring the bottle’s contents. But Pavel Matousek of the Central Laser Facility at the Rutherford Appleton Laboratory in England and his team figured out a way to ignore this glare.
Regular Raman light is focused, hitting only about a millimeter’s worth of sample, and the emitted signal is collected from this illuminated zone. But Matousek and colleagues record a signal from a region offset by 5 to 10 millimeters from where the laser light is focused. This signal comes from photons that migrated into the bottle and through the sample. As with regular Raman, when these photons interact with the sample, they send out photons of a different color.
This setup evades the glare of focused central light. “It’s like shutting off the sun so you can see the stars,” Matousek says.
Since developing this technique, called Spatially Offset Raman Spectroscopy or SORS, in 2005, Matousek’s team has tested it with both tablets and capsules in several types of packaging. While a bottle or blister pack distorted a regular Raman signal, SORS revealed active ingredients in four different meds through their containers, including Sudafed capsules and Nurofen caplets (a brand of ibuprofen), Matousek and Rutherford colleague Charlotte Eliasson reported in Analytical Chemistry in 2007.
Matousek and others are now fiddling with the lasers and data collection to assess liquids through bottles. Once refined, the method could mean that airline travelers will again be allowed to carry on more than 3 ounces of shampoo.
And Matousek and colleagues hope a new version of SORS, described in Chemical Science earlier this year, could allow bone and tissue to be probed, perhaps identifying tumors without invasive biopsies. That approach introduces metal particles to the sample before bombarding it with light.
Mapping meds
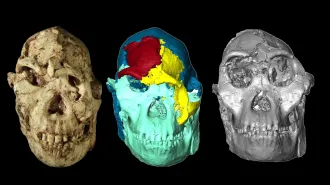
Beyond determining what’s in a sample, some methods can also reveal where. By combining existing spectroscopy with a microscope, camera and some heavy mathematical analyses, researchers can get a pixelated picture of ingredients’ distributions in a pill with stunning detail.
In an early use of one such imaging technique, researchers with the U.S. Food and Drug Administration compared medications bought online with versions from local suppliers. Tickling the samples with near-infrared light, an approach similar to Raman spectroscopy, the team integrated information about absorbed photons with images of the drug itself and some serious number crunching. The near-infrared (or NIR) method showed that the ingredients were poorly mixed in some online versions, the team reported in the International Journal of Pharmaceutics in 2005.
“NIR imaging is slow, but you get a fantastic amount of information,” says Anthony Moffat, former head of the Center for Pharmaceutical Analysis at the University of London.
More recently, Fernández and colleagues from Georgia Tech and France screened antimalarials using several techniques, including a version of DESI that incorporates imaging technologies. Not only did the analysis reveal that some counterfeit antimalarials were chock-full of acetaminophen, but this amped-up DESI also showed that the painkiller was very evenly distributed in the fake tablets, suggesting a fairly sophisticated operation, the team reported in Analytical Chemistry in 2009.
Knowing how well-mixed a counterfeit’s ingredients are might point law enforcement to counterfeiters with high-end equipment who know what they are doing versus a ramshackle setup in a garage. If chemical maps show specks of an active ingredient that appear only on the surface, that might suggest that the pills were pressed in machinery typically used for genuine drugs.
Though such intelligence can help crime fighters bust counterfeiters, many researchers are more concerned with preventing bad meds from getting to patients. Such prevention requires not just new fancy science, but also people and money directed at the right places, says Newton, a leader in the push to deal with counterfeit antimalarials.
In all of Africa, only three countries have labs with the analytical tools needed to monitor the supply chain the way the FDA does in the United States, Newton notes. “There’s more awareness now than 10 years ago, but that awareness hasn’t been translated into interventions and people dealing with the problem,” he says.
Researchers are making headway, though, in the development of portable devices that can be brought out of the lab to the places where people are getting their meds. China has taken NIR spectroscopy mobile, outfitting more than 300 vans with units for screening drugs at local clinics and drugstores in rural regions. There are also compact and portable — though still expensive — Raman devices that make for quick detection by nurses in remote locations. Fernández and colleagues have been working on a portable DART unit, which they described in Analytical Chemistry earlier this year.
“What I would really like to see is a nurse in a clinic in the middle of nowhere being able to put a tablet in a handheld device and be told, ‘You are good to go,’ or ‘No, it is fake,’ ” Fernández says. “The most important thing is to preserve the health of the patient.”